OP04 Long-term outcomes after ileocolonic resection in Crohn’s disease according to the severity of early endoscopic recurrence
N. Hammoudi1, C. Auzolle1, M.L. Tran Minh1, G. Boschetti2, M. Bezault3, A. Buisson4, B. Pariente5, X. Treton6, P. Seksik7, M. Fumery8, L. Le Bourhis9, S. Nancey2, M. Allez1, REMIND Study Group
1Department of Gastroenterology, APHP Saint Louis, Paris, France, 2Department of Gastroenterology, Hospices Civils de Lyon, Lyon, France, 3REMIND, Group, Paris, France, 4Department of Gastroenterology, CHU Clermont-Ferrand, Clermont-Ferrand, France, 5Department of Gastroenterology, Hôpital Claude Huriez, Lille, France, 6Department of Gastroenterology, APHP Hôpital Beaujon, Clichy, France, 7Department of Gastroenterology, APHP Hôpital Saint-Antoine, Paris, France, 8Department of Gastroenterology, CHU Amiens, Amiens, France, 9INSERM, Unité 1160, Paris, France
Background
Early ileocolonoscopy within the first year after surgery is the gold standard to evaluate post-operative recurrence after ileocolonic resection for Crohn’s disease (CD). The aim of the study was to evaluate the association between lesions at ileocolonoscopy 6 months after surgery and long-term outcomes.
Methods
The REMIND group conducted a prospective multicentre study. Patients operated for ileal or ileocolonic CD were included. An ileocolonoscopy was performed 6 months after surgery. An endoscopic classification separating anastomotic and ileal lesions was built (Ax for anastomotic lesions; Ix for neo-terminal ileum lesions evaluated according to the Rutggerts score). Clinical relapse was defined by CD-related symptoms confirmed by imaging, endoscopy or therapeutic intensification, CD-related complication or subsequent surgery.
Results
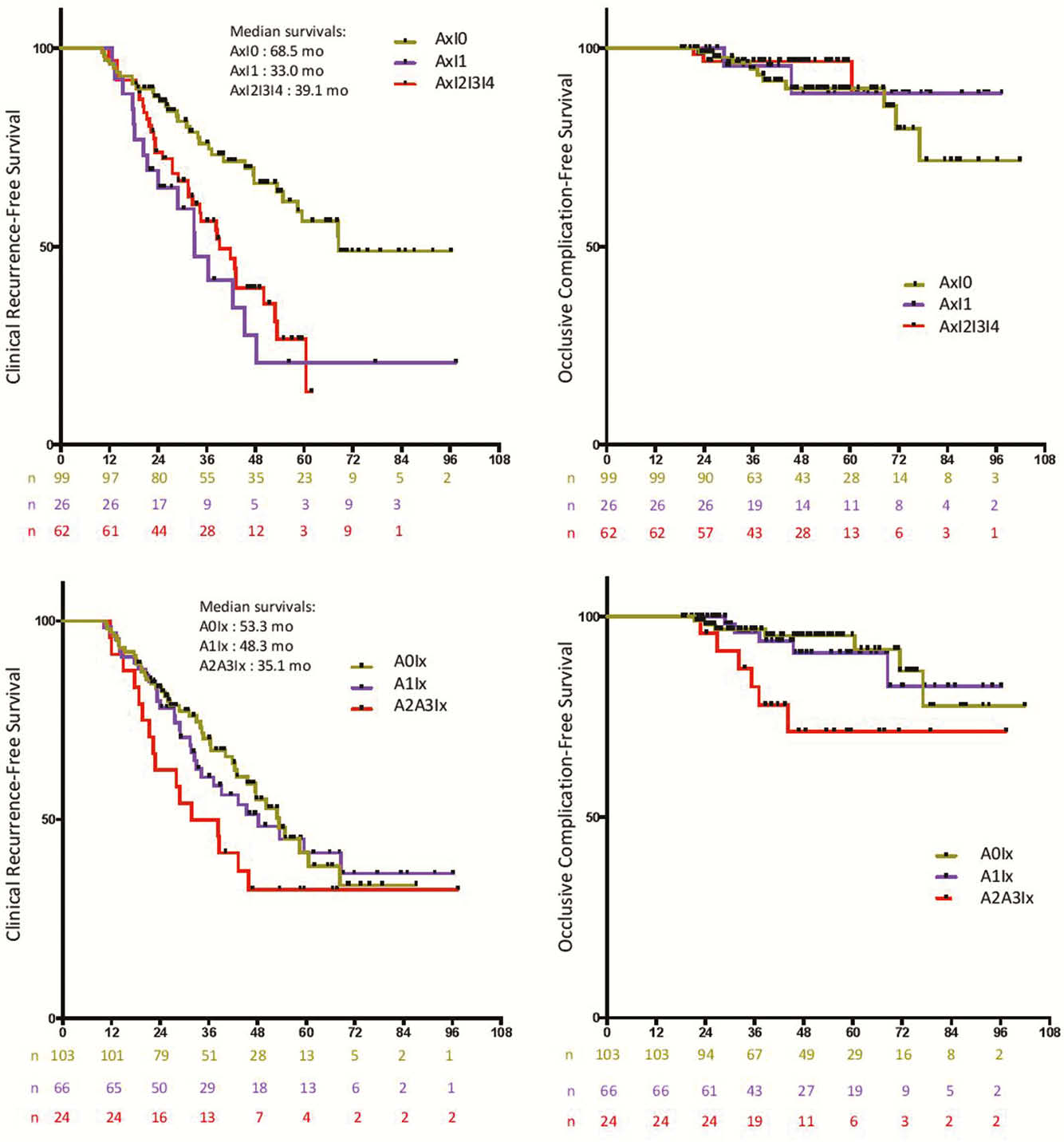
A total of 225 patients were included. Long-term data were available for 193 patients (86%). Median follow-up was 3.82 years (IQR:2.56–5.41) from surgery. Median clinical recurrence-free survival was 47.6 months. Clinical recurrence-free survival was significantly shorter in patients with ileal lesions at early post-operative endoscopy whatever their severity (I1 or I2I3I4) compared with patients without (I0) (median survivals: 68.5, 33.0 and 39.1 months, respectively, for I0, I1 and I2I3I4; I0 vs. I2I3I4:
Conclusion
A classification separating anastomotic and ileal lesions might be more appropriate to define post-operative endoscopic recurrence. Patients with ileal lesions, including mild ones (I1), could beneficiate from treatment step up to improve long-term outcome.


