Outcomes in IBD surgery: Are they adequate?
Alaa El-Hussuna, S-ECCO Committee Member
|
Alaa El-Hussuna |
Are we measuring postoperative outcomes that reflect the success of surgical intervention? Are those outcomes sufficiently sensitive to measure the success of surgical intervention? Complication rate, quality of life and disease relapse are frequently used outcome measures but they have drawbacks that must be taken into consideration. Combining these outcomes with objective measurements will provide the best account of the success of a surgical intervention. Why is this important? Because the greater the number of successful surgical interventions, the lower will be the threshold for accepting surgery as part of the treatment strategy in IBD. Lowering the threshold for acceptance of surgical intervention will convince more gastroenterologists to refer patients to surgery and will eventually enable more patients to benefit from early surgery.
Outcome measures and their limitations
Complication rate
The most frequently used outcome measure is complication rate, which forms an outcome set when used in combination with re-operation rate and re-admission rate. This outcome set sheds light on mission success from the surgeon’s point of view. A low complication rate, absence of need for re-operation and a low re-admission rate can be considered indicators of a successful intervention, i.e. “mission accomplished”. However, deeper examination reveals many flaws in this conception:
1. It has limited sensitivity because the complication rate typically captures only certain measurable adverse events, such as infections and bleeding. It may not be sensitive to more subtle or longer-term issues, such as delayed recovery, minor complications that go unreported or the broader impact on a patient’s overall health and quality of life.
2. It has limited accuracy because of variable reporting [1]. The accuracy of the complication rate can vary significantly depending on how data are collected, recorded and reported. Some complications may be underreported, particularly if they are managed outside of the hospital or are considered less severe. More important is definition variability as different studies define complications differently, leading to inconsistent measures of this outcome. Surveillance bias also limits accuracy as the rate of detected complications can be influenced by the intensity of monitoring and follow-up. More rigorous postoperative surveillance may lead to higher reported complication rates, which may reflect more thorough detection rather than poorer surgical quality.
3. The clinical relevance of complication rate is context dependent. The significance of the complication rate depends on the type of IBD surgery and the patient population [2]. For example, a high complication rate may be more acceptable in a high-risk surgery in a critically ill patient than in an elective, low-risk procedure.
Given these limitations, the complication rate alone does not provide a full picture of surgical success.
Quality of Life
By “quality of life” (QoL), we refer to the impact of surgery on the patient’s overall well-being, including symptom relief and ability to engage in daily activities. QoL is generally considered a more sensitive and comprehensive outcome measure than the complication rate, particularly in the context of chronic conditions like IBD. This is because:
1. It has better sensitivity due to a holistic approach whereby QoL captures a broad range of factors affecting a patient’s well-being, including physical health, psychological state, social relationships and functional abilities. Being responsive to small changes, QoL assessment can detect subtle improvements or declines in health that may not be apparent through standard clinical evaluations.
2. It offers better long-term accuracy due to the possibility of longitudinal tracking. QoL can be measured over time, providing a more accurate picture of the long-term impact of surgery. It captures both immediate postoperative effects and long-term outcomes, which can be particularly important for chronic conditions like IBD.
But QoL, while comprehensive and patient-centred, is a subjective measure and can be influenced by a variety of factors beyond the direct outcomes of surgery:
1. QoL is inherently subjective because it is based on a patient’s personal experience and perception of their health and life. Two patients with similar clinical outcomes may report very different QoL due to differences in their expectations, coping mechanisms, mental health or social support systems. Emotional and psychological states play a detrimental role in QoL measurement. Factors such as depression, anxiety and stress can significantly influence how a patient perceives their QoL. A patient who is clinically well may report a low QoL if they are struggling emotionally, while another with ongoing physical challenges may report a high QoL if they have a positive outlook and strong support.#
2. QoL can be shaped by external factors such as socioeconomic status, access to healthcare, family support and work environment. For example, a patient with good social support and financial stability may report a higher QoL post-surgery than someone facing social isolation or financial hardship, even if their clinical outcomes are similar. Cultural values and norms can also influence how patients perceive and report their QoL. In some cultures, there may be a tendency to underreport problems due to stigma or to overstate well-being to align with social expectations.
3. There are challenges in the measurement of QoL due to variability in the tools used for this purpose. Many tools are available for measuring QoL in IBD, including the Short Form Health Survey (SF-36), EQ-5D and disease-specific instruments such as the Inflammatory Bowel Disease Questionnaire (IBDQ). These tools vary in what they measure and how they weigh different aspects of QoL, which can lead to variability in results. Another subtle but important challenge in QoL measurement is time and context sensitivity: the fact that QoL can fluctuate over time makes it sensitive to when the measurement is taken. For example, a patient’s QoL may be lower immediately after surgery due to recovery challenges but improve significantly over time.
Disease relapse
There are many types of disease relapse after IBD surgery: clinical, endoscopic, biochemical, radiological, histological and surgical [3].
Disease relapse is generally sensitive to changes in disease activity and is typically defined by clear clinical criteria, such as the return of symptoms, endoscopic findings or the need for additional treatment (e.g. steroids, biologics). This gives it a relatively high sensitivity in detecting the recurrence of disease. However, although disease relapse is an objective measurement, it is not fully comprehensive because its accuracy can be influenced by the way in which relapse is defined and detected. For example, some patients may have subclinical disease activity which is not immediately detected but still indicates a form of relapse. Variable definitions of disease relapse can affect the accuracy and comparability of relapse rates. Moreover, disease relapse is time dependent as the timing of follow-up assessments plays a crucial role in the accuracy of measuring relapse. Relapse rates can appear different depending on how long and how frequently patients are monitored. In addition to this, the rate of relapse can be influenced by postoperative management strategies, such as the use of maintenance therapy (e.g. immunosuppressants, biologics). Thus, relapse rates may reflect not only the surgery itself but also the effectiveness of postoperative care.
What is the optimal method of measuring outcomes in IBD surgery then?
A team of researchers from OpenSourceResearch, a non-profit research organisation [4], is working on building a holistic outcome measure by combining complication rate, disease relapse, QoL and
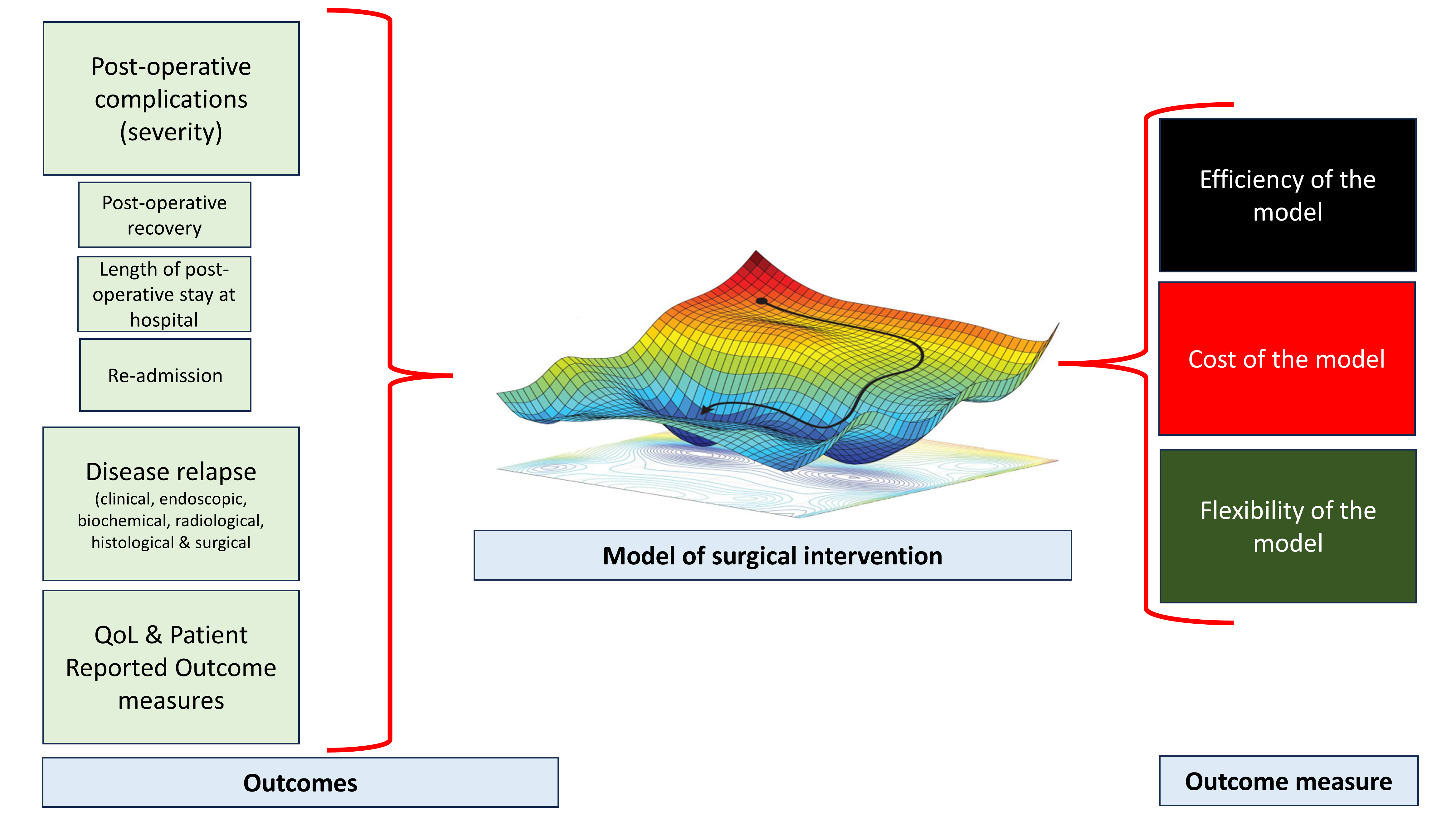
Figure 1 shows a diagram of the OSRC-proposed model, which combines different outcome measures using machine learning to build a holistic outcome measure. The result is an outcome that can be fine-tuned to increase efficiency, improve flexibility and decrease costs.
other outcomes using machine learning (Figure 1). The model will be based on combining different pre-, intra- and postoperative inputs with complementary outcome measures to fully understand the impact of surgery on a patient’s life. This multidimensional approach will provide a more nuanced and accurate picture of a patient’s health.
However, this data-driven model requires integration of data reporting and collection. Can ECCO lead the way through its international database, UR-CARE?
References
- Baker DM, Folan AM, Lee MJ, Jones GL, Brown SR, Lobo AJ. A systematic review and meta-analysis of outcomes after elective surgery for ulcerative colitis. Colorectal Dis 2021;23:18–33. doi: 10.1111/codi.15301.
- Open Source Research Collaborating Group (#OpenSourceResearch). Biological treatment and the potential risk of adverse postoperative outcome in patients with inflammatory bowel disease: an open-source expert panel review of the current literature and future perspectives. Crohn's & Colitis 360, Volume 1, Issue 3, October 2019, otz021. https://doi.org/10.1093/crocol/otz021
- Gisbert JP, Marín AC, Chaparro M. Systematic review: factors associated with relapse of inflammatory bowel disease after discontinuation of anti-TNF therapy. Aliment Pharmacol Ther 2015;42:391–405. doi: 10.1111/apt.13276. Epub 2015 Jun 15. PMID: 26075832.
- https://osrc.network/
