Terra Incognita – for explorers in IBD - Tillotts Pharma Educational Parallel Symposium
 © Tillotts |
The satellite symposium sponsored by Tillotts Pharma was introduced by the Chair, Brian Feagan, Robarts Research Institute, Canada. The topics discussed were of unknown territory in areas where little research has been conducted up until now.
Disclaimer: The views and opinions expressed are those of the speakers and not necessarily of Tillotts Pharma. The satellite symposium is not affiliated with the European Crohn’s and Colitis Organisation (ECCO). The article was created by Tillotts Medical Affairs.
 Tillotts Symposium 2020 © Tillotts |
Patient Preference: Exploring Patients’ Expectations
Peter Lakatos, McGill University Health Center, Canada
Peter Lakatos commenced his talk by highlighting that patients’ and physicians’ expectations in terms of treatment objectives are not aligned. Physicians tend to consider Inflammatory Bowel Disease (IBD) in terms of the medical aspects, e.g. the disease course, medication, complications and treatment outcomes. However, IBD is not necessarily just a disease of the gut; the patient has many other concerns regarding his/her disease and its treatment. Patients’ expectations throughout the course of their IBD diagnosis and treatment journey are summarised below.
Patients’ global expectations
The most important treatment objectives from patients’ perspective are improvement in quality of life (40.2%) and complete resolution of symptoms (33.3%). The symptoms that patients consider most important when prioritising their control are abdominal pain (23.1%) and bowel movement urgency (17.1%) [1]. This was reiterated in a recent study by Boeri in which patients with moderate-to-severe Ulcerative Colitis (UC) considered symptom control to be 2.5 times as important as time to symptom improvement [2].
Patients’ expectations at diagnosis
At the time of diagnosis, patients actively seek shared decision-making and information.
Education of patients is also important: In a web intervention study, 333 patients with mild–to-moderate UC on 5-ASA treatment were randomised to a web group where they received disease-specific education and self-treatment. Adherence to 4 weeks of acute treatment increased by 31% in Denmark and 44% in Ireland compared to the historical control groups. This demonstrates the importance of providing information and empowering patients [4].
Patients seek information: A survey to explore patients’ expectations (n=728) in an IBD cohort in Switzerland revealed that on average, 47% of patients sought information, regardless of the disease stage, with 27% of them being dissatisfied with the information they received at the time of first symptoms. This highlights the importance of making time for the newly diagnosed patient. Not surprisingly, patients’ needs change throughout the disease course, for example, during flares, 43% sought information about drugs and therapies, whilst for those in remission, 57% were interested in research and developments [5].
Preferred source of information: In a population-based Canadian IBD cohort questioned over the acceptability of a variety of information sources, patients indicated that a wide range of information sources would be very acceptable, including brochures/booklets, family doctor and recommended websites. However, the highest ratings were for medical specialists, i.e. the treating physician [6].
Patients’ treatment: back to normal
During therapy: There are the three main topics that patients seek information with regard to treatment; efficacy, side-effect profile and convenience. In a survey of 100 Canadian UC patients, speed of symptom relief was the most important medication attribute (preferred 84% of the time), followed by few side effects (preferred 74% of the time). All other medication attributes were rated as less important, including cost⁄formulary coverage, once-daily dosing and number of pills per dose, which were selected as most important only 36%, 35% and 21% of the time, respectively [7].
When asked to describe their ideal treatment, patients considered high efficacy (97%), lack of side effects (74%), non-parenteral dosing (46%), non-rectal dosing (36%), low cost (23%), fewer pills (23%) and less frequent dosing (23%) as ‘very important’. This study also demonstrated that continuous symptomatic remission is central to patient satisfaction [8].
Patient preference: In a discrete-choice experiment conducted to estimate preferences for 5-ASA treatment in mild-to-moderate UC patients residing in the United States, United Kingdom, Germany and Canada, patient preference varied from country to country. Patients living in the United Kingdom significantly preferred convenience attributes, such as the number of pills taken and ease of swallowing medication. In contrast, patients living in Germany significantly preferred clinical attributes such as flare risk and symptom control, rather than convenience benefits [9].
Conclusions: Peter Lakatos concluded that patients’ top priorities include symptomatic control, access to information and shared decision-making. In terms of therapy, patients’ expectations include symptom control accompanied by few side effects. Patients’ needs change throughout the duration of the disease course and optimisation of medical therapy and self-management is important during remission.
IBDU: The patient who seems to not exist
Johan Burisch, Hvidovre Hospital, Denmark & Richard Russell, Royal Hospital for Children Glasgow, United Kingdom
The second part of the talk focussed on the sometimes forgotten patient. IBD is the umbrella term commonly used to describe UC and CD; the most common forms of IBD. However, there is a small percentage of patients who have disease features of both of these disease forms and are thus classified as having Inflammatory Bowel Disease Undefined (IBDU). The following describes proposed definitions, prevalence, diagnostics, treatment options and disease course of IBDU in adults and children.
IBDU and adults (Johan Burisch, Hvidovre Hospital, Denmark)
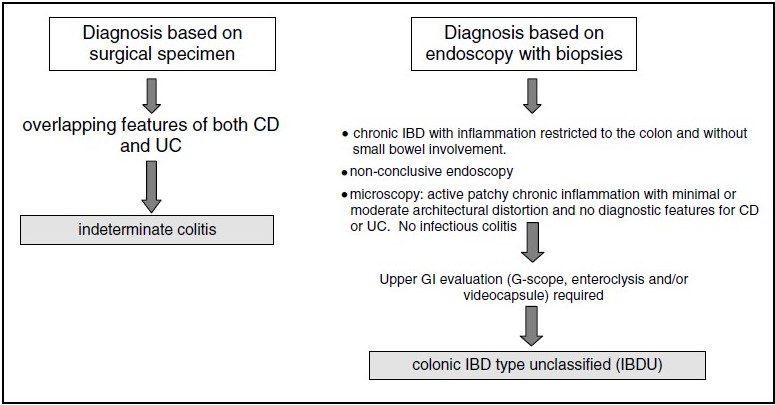
Definition: Currently, no gold standard definition of IBDU exists; in 2004, a Working Party at the Montreal World Congress of Gastroenterology defined indeterminate colitis and IBDU as follows [10].
|
|
Prevalence: Johan Burisch went on to explain that little is known about this patient population. In most epidemiological studies, IBDU patients are often grouped with UC patients and, like proctitis patients, are excluded from clinical trials. IBDU may be more prevalent than one realises. A meta-analysis of 18 studies in adults revealed an IBDU frequency of approximately 6.2% [11].
Disease location: The vast majority of IBDU patients have chronic disease, with the vast majority UC-like in nature; they have an inflamed colon. However, in approximately 60% of patients, it was the histology report that hampered the firm diagnosis of definite UC [12].
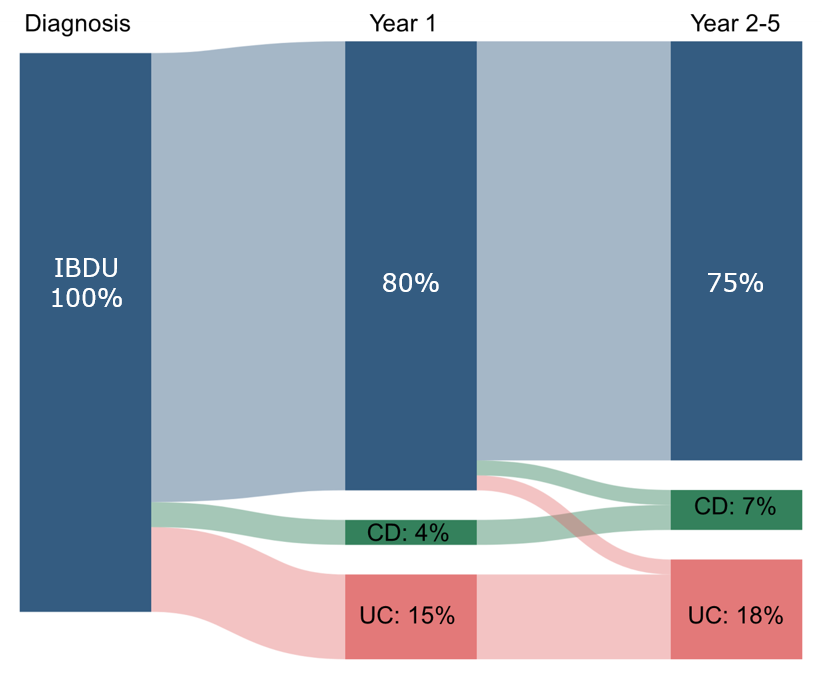
Disease progression: A lot of cases of IBDU eventually evolve into UC or Crohn’s Disease (CD), but a substantial number of patients remain with a diagnosis of IBDU [12]. In the Epi-IBD study cohort, a prospective population-based inception cohort of 1289 IBD patients, 112 were diagnosed with IBDU in centres across Europe. Following 5 years of follow-up, the diagnosis of 28 (25%) patients changed to either UC (n=20, 71%) or CD (n=8, 29%), while 84 patients (75% of the total cohort) remained diagnosed as IBDU [12] – see Figure 1.
Figure 1: Distribution of disease activity in IBDU patients during 5 years of follow-up [12]
|
|
Diagnostic investigations: At diagnosis, all IBDU patients had a lower GI endoscopy performed [colonoscopy (77%) and/or sigmoidoscopy (34%)]. However, following diagnosis and during the 5 year Epi-IBD observation period, 52 (46%) patients underwent no additional investigations and only 54 (48%) had a lower GI endoscopy. All patients in whom the diagnosis was changed during follow-up underwent a lower GI endoscopy [colonoscopy (50%) and/or sigmoidoscopy (54%)], compared to 32 (29%) of patients who continued to be classified as having IBDU (p<0.01) [12].
IBDU treatment: Most patients in the Epi-IBD cohort (n=107, 96%) had a treatment similar to UC patients and received 5-ASA, while 11 (10%) patients received biologics, of whom five remained classified as IBDU throughout the observation period [12]. The disease course of adult IBDU patients was on average mild and the medication burden, including the use of biologics, was low [12].
IBDU and children (Richard Russell, Royal Hospital for Children Glasgow, United Kingdom)
The final part of the symposium, presented by Richard Russell, focussed on the paediatric perspective on IBDU.
Prevalence: Analysis of epidemiological data from 14 studies (n=6262; ten prospective and four retrospective) comparing indeterminate colitis, UC and CD in paediatric populations revealed an IBDU prevalence of 12.7% [11]. IBDU is twice as common in children as in adults.
Genetics: More recently, a genotype association study showed the positioning of the intermediate phenotypes (ileocolonic CD and IBDU) between ileal and colonic CD and between UC and colonic CD, respectively. The study concluded that disease location is in part genetically determined, and the major driver of changes in disease behaviour over time [13].
Diagnostics: The ESPGHAN Revised Porto Criteria for the Diagnosis of Inflammatory Bowel Disease in Children and Adolescents recommend that accurate diagnosis of IBD should be based on a combination of history, physical and laboratory examinations, oesophagogastroduodenoscopy and ileocolonoscopy with histology, and imaging of the small bowel. It is critical to exclude enteric infections [14].
IBD classification algorithms: In order to categorise IBD disorders, the Paediatric IBD Porto Group of ESPGHAN incorporates 23 features into three classes (I, II, III) based on hypothesis-driven analysis – according to their prevalence in UC. According to the algorithm, the disease should be classified as UC if any features of the three classes are lacking. When at least one feature exists, different combinations classify the disease into atypical UC, IBDU or CD. The algorithm differentiates UC from CD and IBDU with 80% sensitivity (95% confidence interval [CI] 71%–88%) and 84% specificity [77%–89%], and CD from IBDU and UC with 78% sensitivity [67%–87%] and 94% specificity [89%–97%] [15].
IBDU treatment: Analysis of a multicentre retrospective longitudinal study of 23 paediatric IBD centres revealed that treatment of IBDU differed from that of UC and CD. On average, in comparison to UC, in IBDU patients there was a lower use of corticosteroids (59% vs 71%; p=0.004) and a higher use of exclusive enteral nutritional (EEN) (10% vs 0.6%; p<0.0001). Similar usage of 5-ASA was observed in the two groups. Whilst compared to patients with CD, IBDU patients received less EEN and immunomodulators (10% vs 37%; p<0.0001 and 26% vs 52%; p<0.0002, respectively), they received more 5-ASA (88% vs 64%; p<0.0001) [16]. The guidance on treatment of patients with IBDU has therefore predominantly been generated by clinical experience. The use of 5-ASA as a first-line treatment for active IBDU was initially used by most physicians.
In summary, IBDU should in general be treated as UC, EEN may be used as a diagnostic challenge (ruling out CD), there is a low threshold for disease reassessment, surgery with pouch is appropriate but should be staged and pouch complications/outcome rates are similar to those in UC.
Disease progression of IBDU patients: IBDU is often viewed as a temporary diagnosis. An analysis of a subset of paediatric subjects from an inception IBD cohort of patients initially enrolled in a prospective multicentre study (the RISK study) was performed. Of the 1411 subjects enrolled, 136 were initially diagnosed with IBDU. Within 2 years of diagnosis, 26% were reclassified as UC and 14% as CD [17]. Thus, 60% of the initial IBDU subjects remained unclassified after 2 years.
Conclusions: Richard Russell concluded that a diagnosis of IBDU is made in around 10% of the paediatric IBD population. A minority of cases can be difficult to subtype, with multidisciplinary teams and IBD classes being the best way to resolve this issue. He recommends initially treating IBDU as UC. Having a firm diagnosis is clearly preferred to guide treatment choices and a better understanding of the nature of IBDU is required.
DISCUSSION
After three interesting and informative talks, the discussion was opened to the audience. The most interesting points that were raised were:
- Patient preference: Patients tend not to inform their treating physicians of their expectations but they do tend to talk to the nurses; hence one can often get extra snippets of important information though this communication route.
- IBDU treatment: Currently no quantitative data are available on treatment success rates in this patient population; however, most patients seem to stay on the initial drug of 5-ASA, with very few needing surgery or step up to biologics.
References
- Casellas F, Herrera-de Guise C, Robles V, Navarro E, Borruel N. Patient preferences for inflammatory bowel disease treatment objectives. Dig Liver Dis. 2017;49:152–6.
- Boeri M, Myers K, Ervin C, et al. Patient and physician preferences for ulcerative colitis treatments in the United States. Clin Exp Gastroenterol. 2019;12:263–78.
- Baars JE, Markus T, Kuipers EJ, van der Woude CJ. Patients' preferences regarding shared decision-making in the treatment of inflammatory bowel disease: results from a patient-empowerment study. Digestion. 2010;81:113–9.
- Elkjaer M, Shuhaibar M, Burisch J, et al., E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided 'Constant-care' approach. Gut. 2010;59:1652–61.
- Pittet V, Vaucher C, Maillard MH, et al. Information needs and concerns of patients with inflammatory bowel disease: What can we learn from participants in a bilingual clinical cohort? PLoS One. 2016;11:1–17.
- Wong S, Walker JR, Carr R, et al. The information needs and preferences of persons with longstanding inflammatory bowel disease. Can J Gastroenterol. 2012;26:525–31.
- Gray JR, Leung E, Scales J. Treatment of ulcerative colitis from the patient's perspective: a survey of preferences and satisfaction with therapy. Aliment Pharmacol Ther. 2009;29:1114–20.
- Loftus EV, Jr. A practical perspective on ulcerative colitis: patients' needs from aminosalicylate therapies. Inflamm Bowel Dis. 2006;12:1107–13.
- Hodgkins P, Swinburn P, Solomon D, Yen L, Dewilde S, Lloyd A. Patient preferences for first-line oral treatment for mild-to-moderate ulcerative colitis: a discrete-choice experiment. Patient 2012;5:33–44.
- Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19 Suppl A:5A–36A.
- Prenzel F, Uhlig HH. Frequency of indeterminate colitis in children and adults with IBD – a metaanalysis. J Crohns Colitis. 2009;3:277–81.
- Burisch J, Katsanos KH, Christodoulou DK, et al. Natural disease course of ulcerative colitis during the first five years of follow-up in a European population-based inception cohort – An Epi-IBD study. J Crohns Colitis. 2019;13:198–208.
- Cleynen I, Boucher G, Jostins L, et al., Inherited determinants of Crohn's disease and ulcerative colitis phenotypes: a genetic association study. Lancet. 2016;387:156–67.
- Levine, A., Koletzko S, Turner D, et al., ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58:795–806.
- Birimberg-Schwartz L, Zucker DM, Akriv A, et al. Development and validation of diagnostic criteria for IBD subtypes including IBD-unclassified in children: a multicentre study from the pediatric IBD Porto Group of ESPGHAN. J Crohns Colitis. 2017;11:1078–84.
- Aloi M, Birimberg-Schwartz L, Buderus S, et al. Treatment options and outcomes of pediatric IBDU compared with other IBD subtypes: a retrospective multicenter study from the IBD Porto Group of ESPGHAN. Inflamm Bowel Dis. 2016;22:1378–83.
- Chandradevan R, Hofmekler T, Mondal K, et al. Evolution of pediatric inflammatory bowel disease unclassified (IBD-U): incorporated with serological and gene expression profiles. Inflamm Bowel Dis. 2018;24:2285–90.