The effects of drug treatment on colorectal mucosal histology
Vincenzo Villanacci, H-ECCO WG Member
 Vincenzo Villanacci Vincenzo Villanacci © ECCO |
The Inflammatory Bowel Diseases (IBD) Crohn’s Disease (CD) and Ulcerative Colitis (UC) are characterised by flares and remission, reflecting the pathological status of the inflamed intestinal tract. For decades, the treatment goal for IBD was the achievement of clinical response or remission. More recently, however, the normalisation of laboratory parameters and intestinal mucosa, termed mucosal healing (MH), has been considered a major target to prevent extra-intestinal complications and achieve sustained clinical remission.
MH, defined as the absence of any abnormality of the intestinal mucosa and normalisation of faecal biomarkers such as faecal calprotectin, has been found to be closely correlated with histological disease activity in both UC and CD and a good predictor of long-term clinical remission. Several trials have shown that anti-TNF-α maintenance therapy is associated with long-term MH in most IBD patients. However, in clinical practice, TNF-α blocking therapy is not prescribed indefinitely, but is usually withdrawn owing to concerns about cost and the fear of long-term side-effects, including in patients with clinical remission. On the other hand, it has been shown that the risk of relapse following withdrawal of infliximab therapy is significant, even in IBD patients with long-standing stable remission: relapse is reported to occur in approximately half of patients within one or two years after withdrawal.
Recently, the term “deep remission” has been applied to patients on immunomodulators or TNF-α blocking therapy or both who have no clinical symptoms and no signs of inflammation (endoscopic remission), but data regarding histology and biochemical markers in IBD patients in deep remission are still scarce.
It has also been argued that the optimal treatment goal is complete resolution of the inflammatory process, in other words histological healing, since endoscopic healing does not necessarily imply that healing is also induced at the microscopic level by the biological drugs. However, the role of histological healing in patients with deep remission has been poorly investigated so far.
Endoscopic Mucosal Healing
In recent years, endoscopic evaluation of MH has become an important endpoint to assess the therapeutic effect of different agents in IBD, especially anti-TNF-α drugs which are able to induce not only clinical remission but also a significant improvement in endoscopic and laboratory parameters.
Unfortunately, controversies regarding the currently available definitions of MH still exist due to the lack of agreement among endoscopists regarding the reporting of endoscopic features and the use of different endoscopic scores to classify disease activity and define MH in UC. These scores are complex, their use is time consuming and there is poor agreement about their cut-off values.
text-align: justify;">Histological Mucosal Healing
At present, histological remission is not recommended as a primary endpoint for therapeutic trials; rather, the suggested endpoint is achievement merely of endoscopic healing. However, as already mentioned, it is of paramount importance to bear in mind that an endoscopic description of MH does not necessarily convey information on histological healing of the mucosa. In fact, several authors have stressed that microscopic evidence of inflammation persists in 16%–100% of patients with endoscopically quiescent colitis. In addition, active histological inflammation has been found to be predictive of clinical relapse during 12 months of follow-up, whereas endoscopic features have not. Therefore, even considering the potential of the new therapeutic approaches, recognition of the importance of achieving histological as well as endoscopic healing might add further value to future trials. On the basis of the available evidence, the optimal treatment goal is complete resolution of the inflammatory process, which requires confirmation by histological assessment. Some points, however, merit discussion.
Firstly, the pre-analytical phase is of paramount importance for correct histological evaluation of MH, as specified in the last ECCO Guidelines: The pathologist should receive an adequate number of biopsies (at least two from each tract), correctly oriented, and obtained from several sites, including the rectum and the terminal ileum. The biopsies should always be accompanied by a report including the age of the patient, clinical information, duration of disease and type of treatment. The histological assessment is usually based on the analysis of several microscopic sections (at least four per slide) stained routinely with haematoxylin and eosin, a cheap and simple technique available in every pathology unit.
A generally accepted definition of histological MH does not exist because of the lack of a standardised approach. Histological healing has been defined by different authors as “a normal mucosa” or as the disappearance of inflammation, and hence, “a mucosa with limited architectural abnormalities but normally differentiated epithelial cells and no signs of active inflammation (presence of neutrophils) or an increased density of lymphocytes and plasma cells”. Several histological scoring systems evaluating both disease activity and MH are available in the literature, such as the Geboes Index and the Robarts and Nancy histopathology indexes.
Most of these indexes are based on the evaluation of various inflammatory features, including the presence of neutrophils in the lamina propria and the epithelium, epithelial cell damage evidenced as loss of cells, mucin depletion, cryptitis, crypt abscesses, erosion and an increase in lymphocytes and plasma cells. Unfortunately, none of these scores are usually utilised in real life because of their subjectivity and complexity.
On the basis of the above considerations, we propose a simplified score based on the evaluation of three simple parameters and the site of involvement.
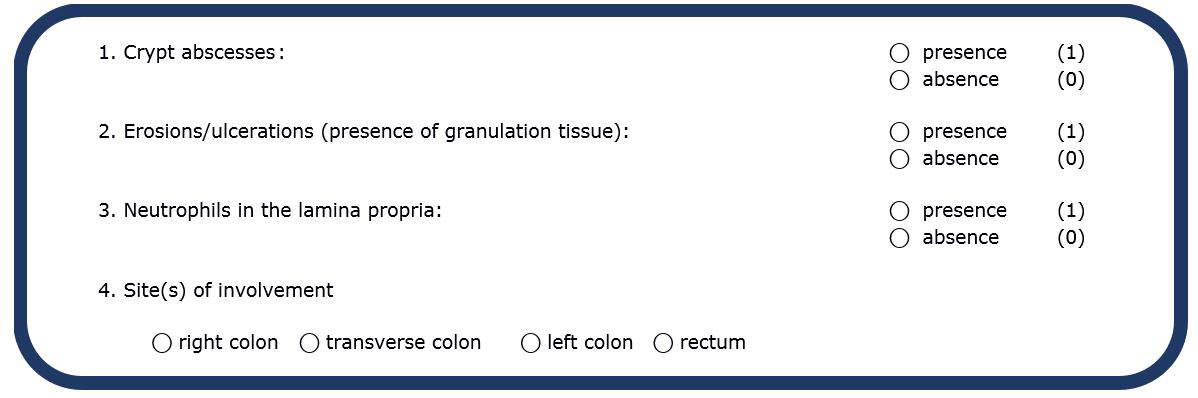
Through the evaluation of the presence/absence of the above morphological features it is possible to avoid the use of grading systems characterised by poor reliability and a high level of subjectivity, thereby achieving better interobserver agreement among pathologists.
References
1. Villanacci, Antonelli, Lanzarotto, Bozzola, Cadei, Bassotti. Usefulness of Different Pathological Scores to Assess Healing of the Mucosa in Inflammatory Bowel Diseases: A Real Life Study. Sci Rep. 2017 Jul 28;7(1):6839.
- Tags: H-ECCO WG