Unveiling the unknown – genetic and environmental risk factors for IBD in Sub-Saharan Africa
Bella Ungar, SciCom Member
 Bella Ungar © ECCO |
The first ECCO Global Grant was awarded at ECCO'24 to an international group leading a fascinating prospective study across Sub-Saharan Africa1. The study is focusing on IBD genetics in the region and is being led by Professor Nick Croft and Dr. Phoebe Hodges from Queen Mary University of London, Professor Paul Kelly and colleagues from the Tropical Gastroenterology and Nutrition Group, University of Zambia and Professor McGovern and his group at Cedars-Sinai, Los Angeles. I had the privilege of discussing aspects of the study with members of the study consortium.
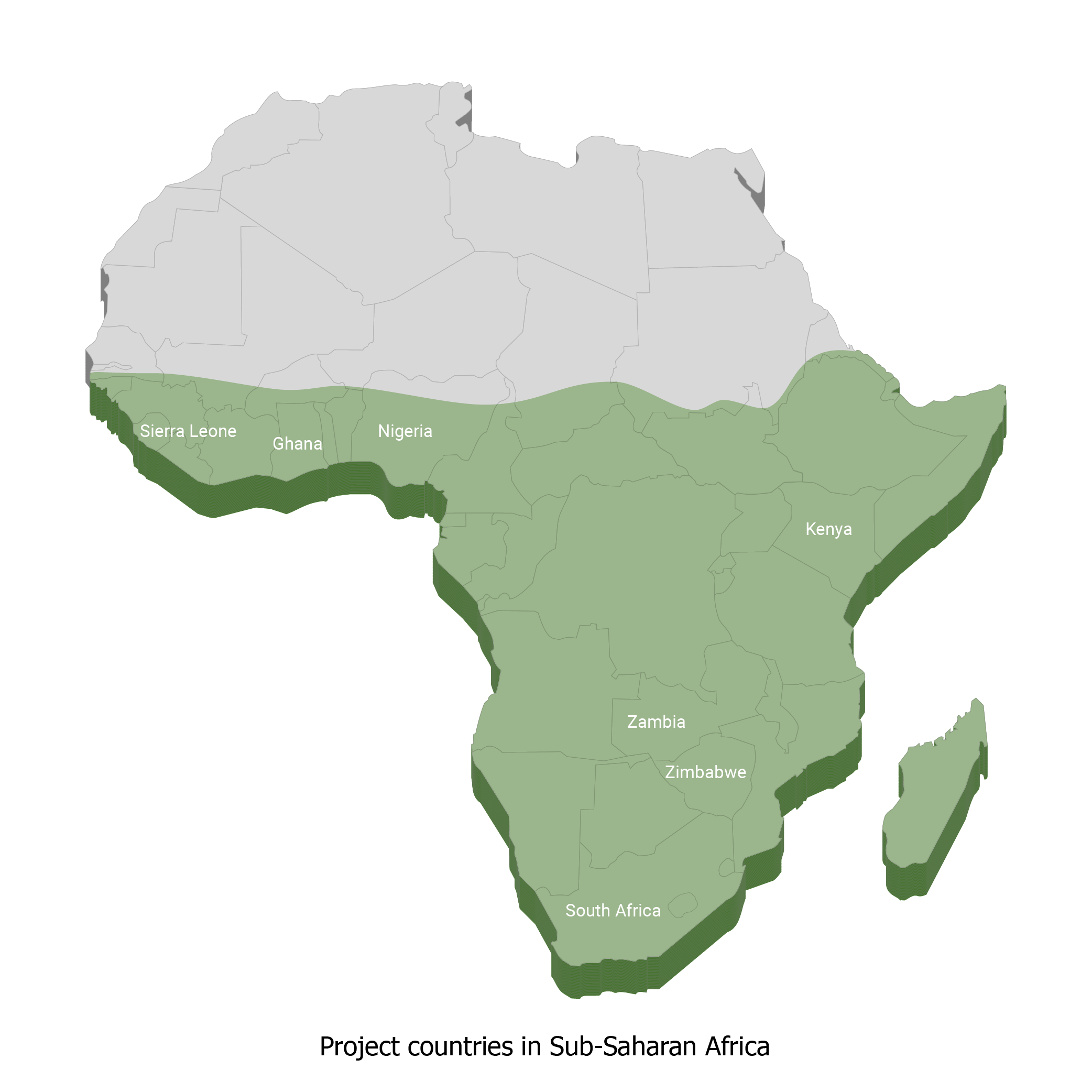
The study was initiated by the African IBD Research Initiative (AIRE), which is an international consortium comprising gastroenterologists, surgeons and pathologists from across Sub-Saharan Africa, including Zambia, Zimbabwe, South Africa, Kenya, Sierra Leone, Ghana and Nigeria, as well as partners from the United Kingdom and North America. In total, ten centres throughout the region are participating in the study.
IBD has traditionally been considered uncommon in Africa. This low incidence has been attributed to reduced environmental exposure on the continent, along with lack of awareness and diagnostics and the significant burden of infectious diseases which present with similar clinical features. In addition, it has been hypothesised that the genetic composition of the population is unique. Genome-wide association studies (GWAS) have significantly improved our understanding of the genetics of diseases, including IBD; however, despite increasing availability of data, much of the heritability and genetics of IBD remains to be explained.
Although evidence is limited, it seems that the incidence of IBD in Sub-Saharan Africa is growing, likely as a result of the rapid demographic transition (urbanisation) and changing environmental exposures. The goal of this year's ECCO Global Grant is to identify genes contributing to the pathogenesis of IBD in Sub-Saharan African populations. Previous genetic studies have primarily focused on high-prevalence regions such as North America and largely European ancestry populations. GWAS have identified more than 240 risk loci in IBD. In patients with Crohn’s Disease (CD) the NOD2 risk alleles were the first identified and most replicated loci. However, this gene has not been universally implicated in IBD, as studies from Asia have not found a significant association. A study on CD in African American patients also suggested that NOD2 variants are not seen in the West African population. Similarly, studies from Tunisia, Morocco and South Africa have not revealed any significant difference between cases and controls with regard to these commonly identified risk alleles. A GWAS in African American IBD patients has identified ‘African-specific’ loci at LSAMP and ZNF649 associated with Ulcerative Colitis which are not seen in patients of European descent. These discrepant findings could have resulted from the small population studied or the lack of other unidentified genes or could imply that genetic factors play a less significant role in certain African populations.
To better understand IBD genetics in their region, the researchers aim to recruit subjects with IBD and non-IBD controls (n=200 in each group) to take part in the study. Clinical data, dietary questionnaires and saliva samples for GWAS analyses will be obtained for each subject. Tuberculosis will be ruled out before study inclusion. It is planned to compare the genetic data with known European ancestry and African American IBD-associated variants. The researchers postulate that genetic differences will be detected in Sub-Saharan African populations and will become even more important in the future due to their interplay with the changing nutrition and demographics.
In addition to contributing to a greater understanding of the pathogenesis of IBD, advances in genetics will hopefully enable specific modifications of IBD therapy in Sub-Saharan Africa, based on the identification, for instance, of variants associated with toxicity to thiopurines or immunogenicity to anti-TNF therapies. Genotypic information could also be combined with clinical data, such as serological markers, in order to predict disease outcomes, e.g. complicated disease and disease requiring surgery.

Global Grant 2024 Project Consortium, Lusaka, Zambia in April 2024.
Meeting received additional funding from the Helmsley Trust.
Picture is subject to copyright © Phoebe Hodges