Update on Non-progressive CD Project
Marieke Pierik, EpiCom Member
 Marieke Pierik © ECCO Marieke Pierik © ECCO |
The Epidemiological Committee (EpiCom) of ECCO promotes epidemiological research within the field of Inflammatory Bowel Diseases (IBD) across Europe. Population-based cohort studies on disease course and prognosis are of great interest for IBD epidemiology since in these cohorts a sample or all of the cases in a defined population are selected for longitudinal assessment of exposure–outcome relationships.
Since Crohn’s Disease (CD) is a heterogeneous disease with wide variations among individuals in terms of severity, phenotype, disease progression (development of strictures or penetrating disease) and therapy response, it is important to include the full spectrum of the disease when evaluating long-term outcome and its predictors. The great advantage of population-based cohorts is the external validity, or applicability of the results to the defined population, and they are therefore ideal for assessment of population attributable risk and risk factors over time, as well as outcomes in CD. Data from population-based cohorts before biologics became widely available showed that a proportion of patients were without disease relapses after 10 years of follow-up (e.g. 10% in the IBSEN cohort, 77% in the European Collaborative Study). Most publications on the long-term outcome of CD, however, focussed mainly on risk factors for recurrent disease or for an unfavourable disease course [defined as a variety of combinations of: disease progression, surgeries, steroid dependency, recurrent courses of steroids or diagnosis of cancer (colorectal cancer or lymphoma)]. The clinical predictors for unfavourable outcome in these studies are present in a large proportion of CD patients and at present are indicative but not sufficient for selection of the optimal treatment strategy for each individual patient.
Therefore the standard treatment strategy at present for CD is step-up therapy with the goal of inducing and maintaining steroid-free clinical remission. However, increasing evidence suggests that early introduction of immunomodulators and/or biologics is associated with an increased probability of endoscopic remission, early sustained remission without steroids and decreased risk of surgery or hospitalisation. Immunosuppressive and/or biologic therapy is associated with an increased risk for (opportunistic) infections and cancer. To prevent over- and under-treatment and to balance the risks and benefits of a treatment strategy, patients should be stratified according to their individual risk. Identification of subgroups of patients not at risk for an unfavourable outcome, and especially those not at risk for an unfavourable outcome without early introduction of immunomodulators and/or biologics, is clinically relevant and EpiCom is currently exploring this issue.
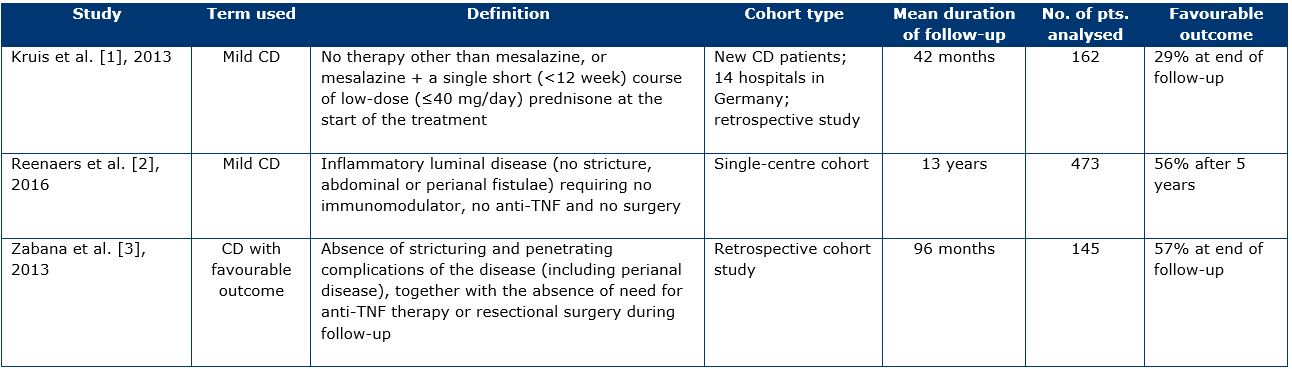
The initial aim of the project is to develop definitions and to explore the validity of these definitions on existing published data sets. In the literature a variety of terms are used to describe CD with a favourable long-term disease course: “mild CD”, “CD with a mild disease course’’, “non-recurrent CD”, “non-progressive CD”, “uncomplicated CD” and “quiescent CD’’. A few cohort studies have focussed specifically on this topic. The definitions used in these trials vary between the studies and are summarised in the table.
EpiCom decided to further use the term non-progressive CD, defined as CD without disease progression (development of stricturing or penetrating disease), perianal complications, surgery or colorectal cancer or intestinal lymphoma after the initial treatment, and without maintenance treatment with immunomodulators and/or biologics or corticosteroids.
An exploratory literature review of population-based cohorts in eras before biologics became widely available showed that 10–25% of CD patients have no recurrence of disease activity after the initial flare-up. A substantial proportion of patients in these cohorts never require corticosteroids or immunomodulators/biologics. These data indicate that a proportion of CD patients can indeed be classified as having the non-progressive CD phenotype. Cumulative relapse rates in population-based cohorts starting in or before the 1990s further show cumulative relapse rates of 34%–53% after 1 year, increasing to 77%–90% after 10 years of follow-up. The cumulative surgical recurrence rates also increase until 10 years after diagnosis, although the increase between 5 and 10 years after diagnosis is less pronounced.
Given the external validity of population-based cohorts for further exploration of the prevalence and identification of clinical risk factors for non-progressive CD, a detailed review of available data sets with more than 5 or, preferably, 10 years of follow-up will be initiated by EpiCom. In the future, proof of concept studies including imaging to assess intestinal damage are warranted.
References
1. Kruis W, Katalinic A, Klugmann T, et al. Predictive factors for an uncomplicated long-term course of Crohn's disease: a retrospective analysis. J Crohns Colitis. 2013;7:e263–70.
2. Reenaers C, Pirard C, Vankemseke C, Latour P, Belaiche J, Louis E. Long-term evolution and predictive factors of mild inflammatory bowel disease. Scand J Gastroenterol. 2016;51:712–9.
3. Zabana Y, Garcia-Planella E, van Domselaar M, et al. Predictors of favourable outcome in inflammatory Crohn's disease. A retrospective observational study. Gastroenterol Hepatol. 2013;36:616–23.
- Tags: EpiCom