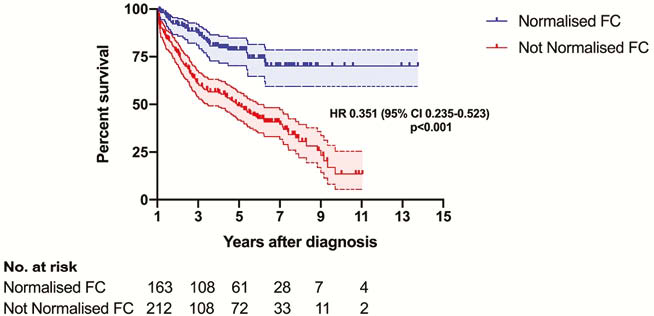
DOP11 Normalisation of faecal calprotectin within 12 months of diagnosis is associated with a reduced risk of disease progression in Crohn’s disease
N. Plevris, J. Fulforth, P. Jenkinson, M. Lyons, C. Chuah, S. Siakavellas, R. Pattenden, I. Arnott, G. Jones, C. Lees
The Edinburgh IBD Unit, Gastroenterology, Western General Hospital, Edinburgh, UK
Background
Faecal calprotectin (FC) demonstrates an excellent correlation with endoscopic inflammation. In addition, a treatment-decision algorithm for Crohn’s disease (CD) incorporating FC outperforms and improves 12-month mucosal healing compared with a strategy based on symptoms alone. The aim of this study was to determine whether normalisation of FC (<250 μg/g) within 12-months of diagnosis is associated with a reduction in disease progression in CD.
Methods
This was a retrospective cohort study performed at a tertiary IBD centre. All incident cases of CD diagnosed between 2005 and 2017 were identified. Patients with an FC measurement of >250 μg/g at diagnosis who also had at least 1 follow-up FC measured within the first 12-months of diagnosis and >12 months of follow-up were included. The primary endpoint was a composite of progression in Montreal disease behaviour (B1 to B2/3 or B2 to B3 or new perianal disease), surgery or hospitalisation.
Results
A total of 375 patients were included with a median follow-up of 5.3 years (IQR 3.1–7.4). Normalisation of FC (<250 μg/g) within 12 months of diagnosis was confirmed in 43.5% (
Conclusion
Normalisation of FC by 12-months of diagnosis is associated with a reduced risk of disease progression in CD. Our data provide strong support for implementation of treat-to-target strategies earlier than previously tested in Crohn’s disease. The immediate implication for healthcare providers and patients is that by ensuring resolution of mucosal inflammation - measured by proxy with faecal calprotectin, and regardless of other variables - within 1 year of diagnosis has a dramatic effect on disease course.


