DOP17 In high-risk Crohn’s Disease patients, anastomosis configuration types have similar rates of endoscopic recurrence
Bachour, S.(1);Shah, R.(1);Lyu, R.(2);Rieder, F.(1);Cohen, B.(1);Qazi, T.(1);Lashner, B.(1);Lipman, J.(3);Regueiro, M.(1);Lightner, A.(3);Holubar, S.(3);Click, B.(1)
(1)Cleveland Clinic Foundation, Department of Gastroenterology and Hepatology, Cleveland, United States;(2)Cleveland Clinic Foundation, Department of Quantitative Health Sciences, Cleveland, United States;(3)Cleveland Clinic Foundation, Department of Colorectal Surgery, Cleveland, United States
Background
There is conflicting data on the influence of surgical anastomosis configuration on endoscopic postoperative recurrence (POR) of Crohn’s disease (CD) following ileocolonic resection (ICR). Furthermore, whether this relationship differs by preoperative risk factors for POR has not been studied. We aimed to assess the role of ileocolonic anastomosis type on the rate and time to POR by preoperative POR risk.
Methods
Retrospective cohort study of adult CD patients who underwent ICR between 2009-2020 at a quaternary IBD referral center. Patients with a primary or secondary anastomosis and ≥1 postoperative colonoscopy were included. Endoscopic activity was assessed by modified Rutgeerts’ scoring. POR was defined as Rutgeerts’ ≥ i2b. Patients were categorized by anastomosis type: end-to-end (ETE), end-to-side (ETS), or side-to-side (STS). High-risk CD patients were defined by ≥1: age ≤ 30 years, active smoker, or ≥2 ICR for penetrating disease.
Results
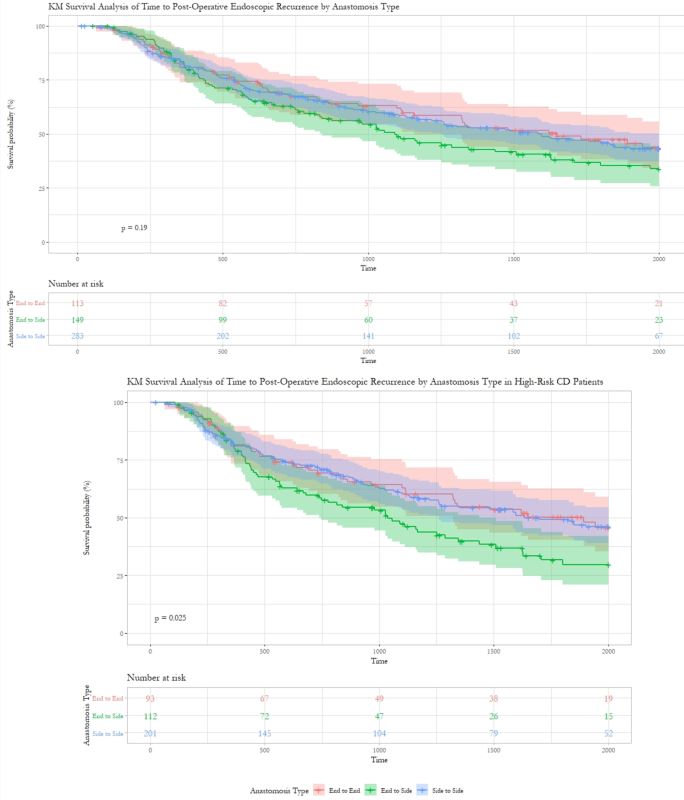
548 CD patients (52.6% female, age 35 y, 15.5% > 1 prior ICR, 19.7% on biologic prophylaxis, 74.8% high-risk for POR) were included in the study (Figure 1). The majority received a STS (52.0%, N=285), 27.2% ETS, and 20.8% ETE. Patients with an ETE were diagnosed with CD at a younger age (p=0.04), had more penetrating disease (p=0.01), hand-sewn anastomoses (p <0.001), and diverting loop ileostomies (p=0.02). There were no differences in prior ICR, smoking, biologic prophylaxis, or in median time from ICR to first post-operative colonoscopy (388.5 days, p=0.41) or POR detection (905 days, p=0.8) by anastomosis type. ETS patients had a shorter median follow-up time (3.9 y, p=0.02). The majority (55.7%) of all patients experienced POR (57% ETS; 55.4% STS; 54.4% ETE). Overall, there was no significant association between anastomosis type and POR rate (p=0.91) or time to POR (p=0.32). However, in high-risk CD patients, ETS was significantly associated with more rapid time to POR on log-rank (p=0.03) and multivariable Cox modeling (HR=1.51; p=0.04). Postoperative prophylactic biologic therapy initiated within 3 months of ICR significantly delayed POR in the overall cohort (HR=0.64; p=0.012) and the high-risk CD subgroup (HR=0.67; p=0.047). High-risk CD patients on prophylactic biologics had no difference in time to POR by anastomosis type (p=0.66).
Conclusion
In post-operative CD patients, there is no difference in rates of endoscopic recurrence by anastomosis configuration regardless of risk stratification. In high-risk patients, ETS was associated with more rapid endoscopic recurrence compared to other configurations, however prophylactic postoperative biologics may protect against this effect.
Figure 2: KM Survival analysis of time (days) to POR