DOP20 Can lifestyle and psychosocial factors predict flares of IBD; an exploratory study using telemedicine
R.C.A. Lalisang1, G. Adriaans2, M. de Jong3, A. van der Meulen-de Jong4, M. Romberg-Camps5, N. Mahmmod6, T. Markus-de Kwaadsteniet7, G. Dijkstra8, J. Haans2, C. Stamm9, R. Vanwersch10, D. Jonkers11, R.J. Almeida12,13, M.J. Pierik2, MyIBDcoach Study Group
1Division of Gastroenterology and Hepatology, Maastricht Universitair Medisch Centrum+, Pacmed, Maastricht, The Netherlands, 2Division of Gastroenterology and Hepatology, Maastricht Universitair Medisch Centrum+, Maastricht, The Netherlands, 3Haga Ziekenhuis, Department of Gastroenterology, Den Haag, The Netherlands, 4Department of Gastroenterology, Leiden University Medical Center, Leiden, The Netherlands, 5Department of Gastroenterology, Zuyderland Medical Centre, Sittard, The Netherlands, 6Department of Gastroenterology, St. Antonius Ziekenhuis, Nieuwegein, The Netherlands, 7Stichting mijnIBDcoach, Board, Mijdrecht, The Netherlands, 8Department of Gastroenterology, Universitair Medisch Centrum Groningen, Groningen, The Netherlands, 9Department of Health Care, Pacmed, Amsterdam, The Netherlands, 10Information Systems, Faculty of Industrial Engineering, Eindhoven University of Technology, Eindhoven, The Netherlands, 11Department of Internal Medicine, Division of Gastroenterology-Hepatology, University Maastricht, Maastricht, The Netherlands, 12Department of Quantitative Economics, School of Business and Economics, Maastricht University, Maastricht, The Netherlands, 13Department of Data Analytics and Digitalisation, Maastricht University, Maastricht, The Netherlands
Background
Tight control of mucosal inflammation and prevention of disease flares are emerging treatment goals to prevent disease progression in inflammatory bowel disease (IBD). The state of the art clinical classification only marginally predict flare occurrence. Mounting evidence shows that psychosocial and lifestyle factors are associated with flares. Longitudinal monitoring of these factors has been made possible by implementing a web-based telemedicine tool, called
Methods
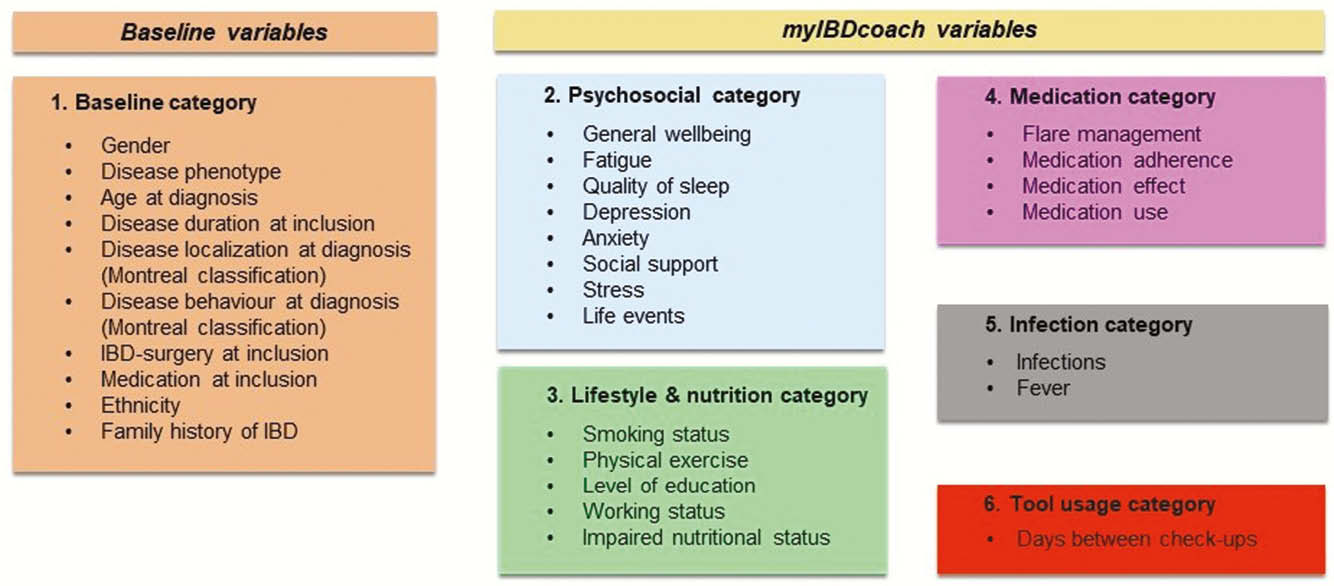
Consecutive IBD patients (
Results
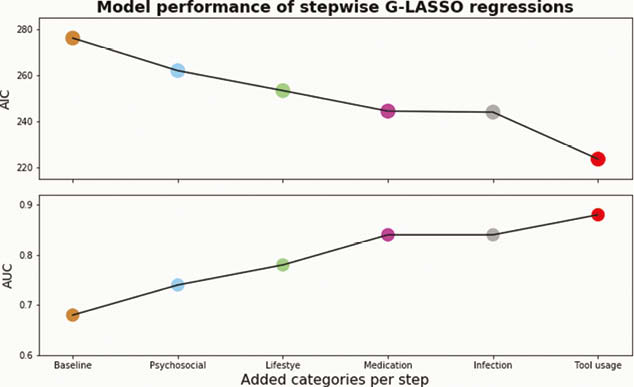
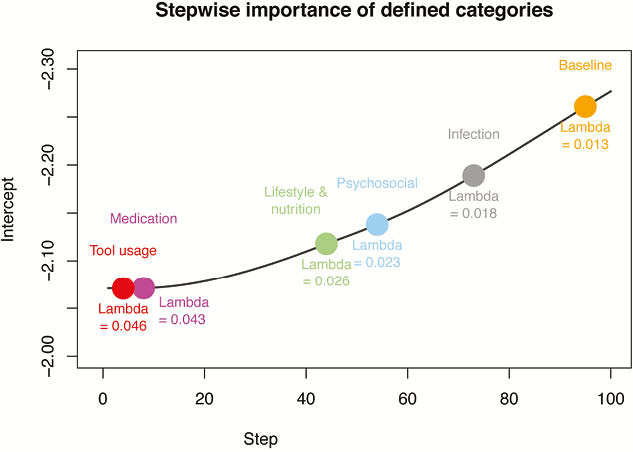
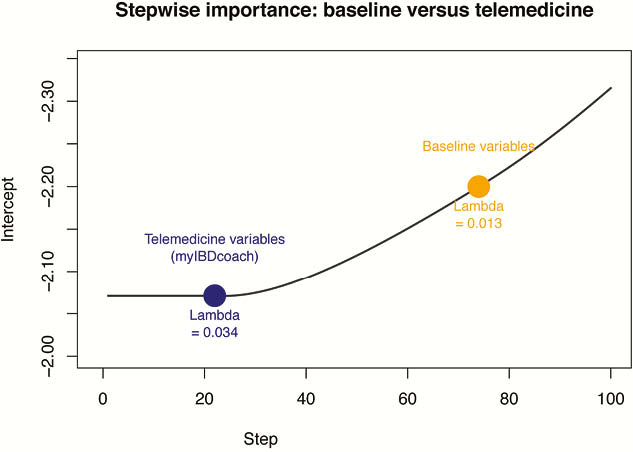
Seven G-LASSO regressions were estimated and evaluated using the Akaike information criteria (AIC), the area under the curve (AUC) and stepwise importance using 10-fold cross-validated penalty parameter. Figure 2 shows that the overall model performance increased when consecutively adding extra variable categories, the largest increase occurred for psychosocial and lifestyle factors. All telemedicine variable categories were found to be more important compared with the baseline variable category, as shown in Figure 3. Results shown in Figure 4 indicate that the information from
Conclusion
In this exploratory study, psychosocial and lifestyle factors monitored via telemedicine are of superior value to predict flares in IBD patients compared with clinical stratification. Holistic monitoring, including psychosocial and lifestyle factors, and targeted interventions are of interest for future trials and are a promising strategy to prevent flares and improve the outcome of IBD.


