DOP22 Clinical, biochemical and endoscopic disease activity of Inflammatory Bowel Diseases are not associated with the severity or long-term outcomes of COVID-19 – A Danish prospective population-based cohort study
Attauabi, M.(1,2,3);Dahlerup, J.F.(4);Poulsen, A.(5);Hansen, M.R.(6);Vester-Andersen, M.K.(7);Eraslan, S.(2);Prahm, A.P.(5);Pedersen, N.(8);Larsen, L.(9);Jess, T.(9,10);Neumann, A.(11);Haderslev, K.V.(12);Molazahi, A.(13);Lødrup, A.B.(14);Glerup, H.(15);Oppfeldt, A.M.(16);Jensen, M.D.(17);Theede, K.(1,3);Kiszka-Kanowitz, M.(1,3);Seidelin, J.B.(2);Burisch, J.(1,3);
(1)Copenhagen University Hospital- Hvidovre, Gastrounit- Medical Section, Hvidovre, Denmark;(2)Herlev Hospital- University of Copenhagen, Department of Gastroenterology and Hepatology, Herlev, Denmark;(3)University of Copenhagen- Hvidovre Hospital, Copenhagen Center for Inflammatory Bowel Disease in Children- Adolescents and Adults, Hvidovre, Denmark;(4)Aarhus University Hospital, Department of Hepatology and Gastroenterology, Aarhus, Denmark;(5)Bispebjerg University Hospital, Digestive Disease Center, Copenhagen, Denmark;(6)North Zealand University Hospital, Department of Gastroenterology, Frederikssund, Denmark;(7)Zealand University Hospital- Koege, Department of Internal Medicine, Koege, Denmark;(8)Slagelse Hospital, Department of Gastroenterology, Slagelse, Denmark;(9)Aalborg University Hospital, Department of Gastroenterology and Hepatology, Aalborg, Denmark;(10)Aalborg University, National Center of Excellence for Molecular Prediction of Inflammatory Bowel Disease PREDICT- Department of Clinical Medicine, Copenhagen, Denmark;(11)Region Hospital Viborg, Department of Internal Medicine, Viborg, Denmark;(12)Rigshospitalet- Copenhagen University Hospital, Department of Gastroenterology, Copenhagen, Denmark;(13)Holbaek Hospital, Department of Internal Medicine, Holbaek, Denmark;(14)Region Hospital West Jutland- Herning, Department of Internal Medicine, Herning, Denmark;(15)Region Hospital Silkeborg, Department of Internal Medicine, Silkeborg, Denmark;(16)Region Hospital Horsens, Department of Internal Medicine, Horsens, Denmark;(17)Lillebaelt Hospital- Vejle, Department of Internal Medicine- Section of Gastroenterology, Vejl, Denmark; Danish COVID-IBD Study Group
Background
Whether the disease activity of ulcerative colitis (UC) and Crohn’s disease (CD) is correlated with the severity of coronavirus disease 2019 (COVID-19) remains poorly investigated with only few selected cohort studies having addressed this in the past.
Methods
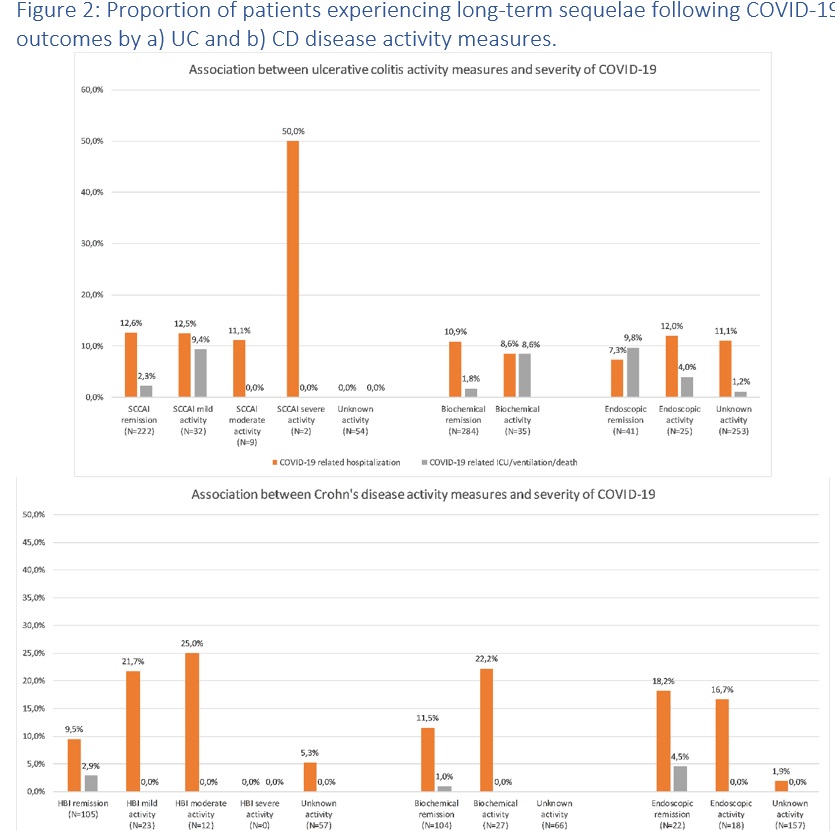
We conducted a population-based study investigating the outcomes of COVID-19 among patients with UC and CD in Denmark. The Danish COVID-19 IBD Database is an extensive population-based database which prospectively monitors the disease course of laboratory-confirmed COVID-19 among patients with UC and CD. Severe COVID-19 was defined as COVID-19 necessitating intensive care unit admission, ventilator use, or death, while adverse COVID-19 was defined as requirement of COVID-19 related hospitalization. Clinical disease activity was measured by simple clinical colitis index and Harvey-Bradshaw Index in UC and CD, respectively. The biochemical activity was defined as C-reactive protein higher than 5 mg/L or fecal calprotectin higher than 250 μg/g. The endoscopic activity was defined as Mayo Endoscopic Subscore of at least 2 in UC, or Simple Endoscopic Score Crohn’s Disease of at least 3 for CD. Sequelae following COVID-19 were defined as symptoms that (i) developed during or after an infection consistent with COVID-19, (ii) and were present for more than 12 weeks, (iii) and were not attributable to alternative diagnoses.
Results
During the inclusion period between January 28th, 2020, to April 1st, 2021, the study included 319 patients with UC and 197 patients with CD who developed laboratory confirmed COVID-19. Of these, data on clinical, biochemical, and endoscopic activity were available among 265/319 (83.1%), 319/319 (100.0%), and 66/319 (20.7%) of patients with UC, respectively, and 140/197 (71.1%), 131/197 (66.5%), and 42/197 (21.3%) of patients with CD. Figures 1-2 outlines the outcomes of COVID-19 according to the degree of clinical, biochemical and endoscopic disease activity. In both UC and CD, clinical, biochemical, and endoscopic activity were not associated with adverse or severe COVID-19, nor long-term outcomes, in unadjusted nor adjusted analysis (Table 1).


Conclusion
In this population-based study, we found no association between disease activity of UC or CD and severity of COVID-19. These findings have implications for the risk stratification of patients with IBD acquiring COVID-19.


