DOP25 Medication use and comorbidities among elderly when compared with younger patients with inflammatory bowel disease in the TARGET-IBD cohort
E. Barnes1, J. Hanson2, M. Regueiro3, S. Saha4, B.E. Sands5, D. Rubin6, M. Dubinsky7, C. Siegel8, D. Gazis9, J. Crawford10, M. Long1
1Department of Gastroenterology, University of North Carolina, Chapel Hill, USA, 2Department of Gastroenterology, Atrium Health, Charlotte, USA, 3Department of Gastroenterology, Cleveland Clinic, Cleveland, USA, 4Department of Gastroenterology, University of Wisconsin, Madison, USA, 5Dr. Henry D. Janowitz Division of Gastroenterology, Icahn School of Medicine at Mount Sinai Medical Center, New York, USA, 6Department of Gastroenterology, University of Chicago, Chicago, USA, 7Department of Pediatric Gastroenterology and Nutrition, Mount Sinai School of Medicine, New York, USA, 8Department of Gastroenterology, Dartmouth Hitchcock, Lebanon, USA, 9Department of Statistics, TARGET PharmaSolutions, Durham, USA, 10Scientific and Medical Affairs, TARGET PharmaSolutions, Durham, USA
Background
When compared with younger patients, much less is known regarding inflammatory bowel disease (IBD)-related medications in the elderly (>65 years) patients. This analysis uses a large cohort of patients with IBD to describe the distribution of patient characteristics and patterns of medication use.
Methods
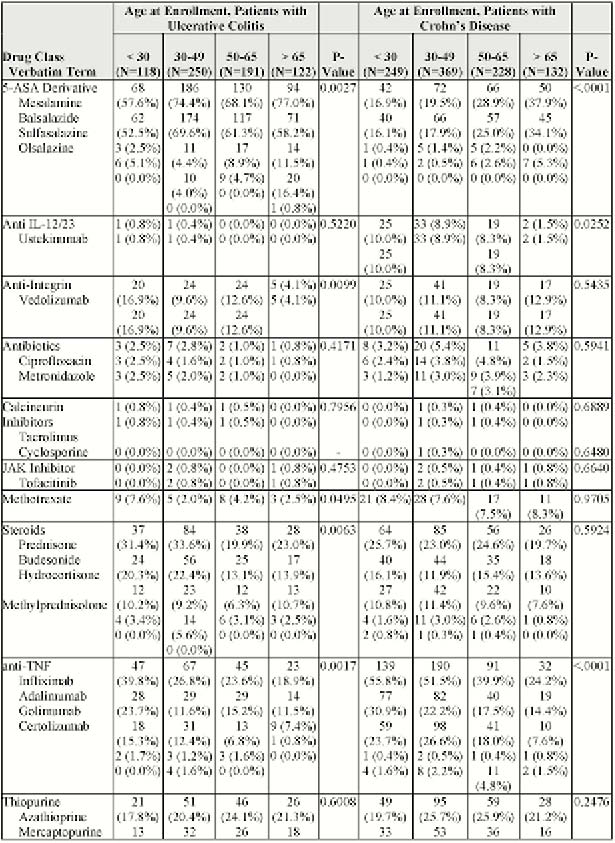
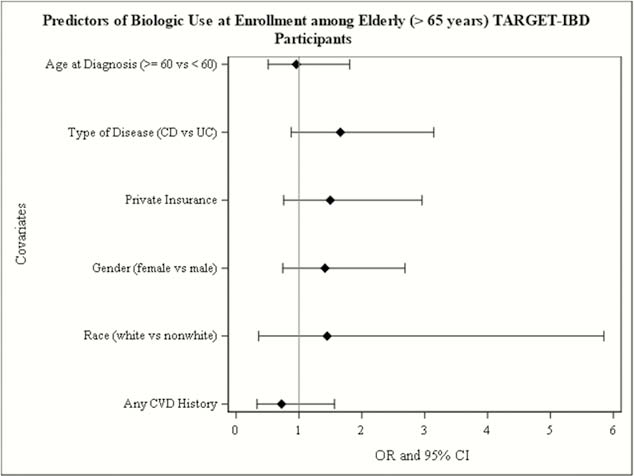
TARGET-IBD is a longitudinal cohort of patients with IBD receiving usual care at community and academic practices in the US. Patients with IBD enrolled between July 2017 and May 2019 were included in this analysis. The prevalence of medication use by drug class at the time of enrolment among patients with both ulcerative colitis (UC) and Crohn’s disease (CD) was estimated. Age was stratified into the following categories: <30, 30–49, 50–65 and >65 years. Proportions and means of patient characteristics were compared using tests of association. The odds of biologic use at enrolment was modelled as was the 95% CI by patient characteristics using logistics regression.
Results
681 patients with UC and 979 patients with CD were included in the analysis. At enrolment, mesalamine was the most common medication used among patients with CD >65 years (34%) and among patients with UC across all age categories (58%–77%, Table 1). The use of mesalamine generally increased with advancing age. Patients with CD >65 years were more than twice as likely to be users of mesalamine at enrolment than patients <30 years (
Conclusion
Elderly patients with IBD, whether those with new diagnoses or individuals with the longstanding disease make up a substantial portion of the IBD population. Given that elderly patients demonstrate significant differences in medication use patterns compared with younger patients with IBD, studies of efficacy and adverse events specific to this population are warranted.


