DOP27 Transanal minimally invasive surgery (TAMIS): A novel approach for treatment of pouch failure
E. Van Praag BSc1, R. Hompes1, C. Buskens1, P. Tanis1, M. Duijvestein2, W. Bemelman1
1Department of Surgery, Amsterdam UMC-location AMC, Amsterdam, The Netherlands, 2Department of Gastroenterology and Hepatology, Amsterdam UMC-location AMC, Amsterdam, The Netherlands
Background
Many different pouch failure (PF) indications and procedures are known. In literature, different types of PF are randomly classified and often stacked together due to complexity. Transanal minimally invasive surgery (TAMIS) is becoming increasingly popular for redo-surgery due to greater accessibility and visibility in complex pelvic surgery compared with the conventional abdominal approach. We aimed to evaluate the efficacy of TAMIS in patients with PF.
Methods
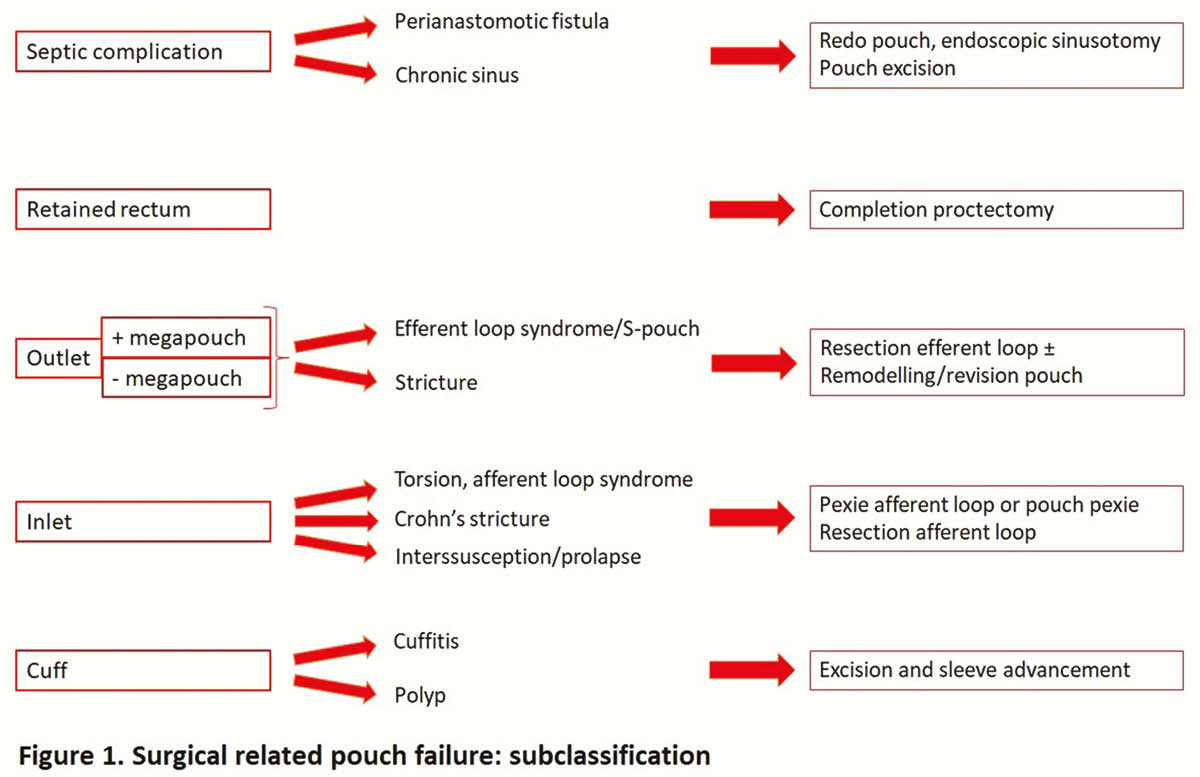
This retrospective study includes all consecutive patients over 18-year old with an ileal pouch-anal anastomosis (IPAA) and PF that were managed with TAMIS between July 2014 and July 2019. Patient characteristics, operative indications, perioperative outcomes and short-term follow-up (FU) are described using a suggested subclassification for surgical-related PF (Figure 1).
Results
Forty-six procedures were completed in 42 patients, predominantly male (66.7%) with a median age of 44.6 (range 22.0–70.8) years. Initial IPAA indications were familial adenomatous polyposis (
Conclusion
TAMIS for PF after IPAA is technically feasible with acceptable short-term outcomes. Peri-operative morbidity is high and reflects the complexity of these procedures. Success after PF procedures is difficult to interpret due to a wide range of possible outcomes such as technical success, conversion rate and number of patients with a permanent stoma. The PF subclassification makes the complex problem and surgical management of PF comprehensible.


