DOP69 Long-term outcome of infantile and very early onset IBD: A multi-center study from the IBD Porto group of ESPGHAN
Guz Mark, A.(1,2);Aloi, M.(3);Scarallo , L.(4);Bramuzzo, M.(5);Escher, J.C.(6);Alvisi, P.(7);Henderson, P.(8);Hojsak, I.(9);Lev-Tzion, R.(10);El-Matary, W.(11);Schwerd, T.(12);Weiss, B.(13);Sladek, M.(14);Strisciuglio, C.(15);Müller, K.(16);Olbjørn, C.(17);Tzivinikos, C.(18);Yerushalmy-Feler, A.(19);Christiaens, A.(20);Norsa, L.(21);Viola, I.(22);de Ridder, L.(6);Shouval, D.(23);Lega, S.(5);Lionetti, P.(24);Catassi, G.(25);Assa, A.(26);
(1)Schneider Children's Medical Center of Israel, Institute of Gastroenterology- Nutrition and Liver Diseases, Petach Tikva, Israel;(2)Tel-Aviv University, Sackler Faculty of Medicine, Tel Aviv, Israel;(3)Umberto I Hospital, Pediatric and Gastroenterology Unit- Sapienza University of Rome, Rome, Italy;(4)Meyer children’s Hospital, Gastroenterology and Nutrition Unit, Florence, Italy;(5)Institute for Maternal and Child Health - IRCCS "Burlo Garofolo", Gastroenterology- Digestive Endoscopy and Nutrition Unit, Trieste, Italy;(6)Erasmus MC-Sophia Children’s Hospital, Department of Pediatric Gastroenterology, Rotterdam, The Netherlands;(7)Maggiore hospital, Pediatric Gastroenterology unit, Bologna, Italy;(8)Royal Hospital for Children and Young People, Department of Paediatric Gastroenterology and Nutrition, Edinburgh, United Kingdom;(9)Children’s Hospital Zagreb, University of Zagreb Medical School, Zagreb, Croatia;(10)Shaare Zedek Medical Center, Juliet Keidan Institute of Pediatric Gastroenterology Hepatology and Nutrition, Jerusalem, Israel;(11)Pediatric Gastroenterology, University of Manitoba, Winnipeg, Canada;(12)Dr von Hauner Children's Hospital- LMU Munich, Department of Pediatrics, Munich, Germany;(13)Edmond & Lily Safra Children's Hospital- Sheba Medical Center and Sackler Faculty of Medicine- Tel Aviv University, Pediatric Gastroenterology Unit, Tel Aviv, Israel;(14)Jagiellonian University Medical College, Department of Pediatrics- Gastroenterology and Nutrition, Krakow, Poland;(15)Department of Woman- Child and General and Specialistic Surgery, University of Campania Vanvitelli, Naples, Italy;(16)Heim Pal National Institute for Pediatrics, Institute for Translational Medicine- Faculty of Medicine- University of Pécs, Budapest, Hungary;(17)Akershus university hospital, Department of Pediatric and Adolescent Medicine, Lørenskog, Norway;(18)Al Jalila Children ‘s Hospital - Mohammed Bin Rashid University, Paediatric Gastroenterology Department, Dubai, United Arab Emirates;(19)"Dana-Dwek" Children's Hospital- Tel Aviv Sourasky Medical Center and the Sackler Faculty of Medicine- Tel Aviv University, Pediatric Gastroenterology Institute, Tel Aviv, Israel;(20)University Hospital Brussels, Pediatric Gastroenterology and Nutrition, Brussels, Belgium;(21)ASST Papa Giovanni XXIII, Pediatric Hepatology- Gastroenterology and Transplantation, Bergamo, Italy;(22)University of Messina, Pediatric Gastroenterology and Cystic Fibrosis Unit- Department of Human Pathology in Adulthood and Childhood "G. Barresi, Messina, Italy;(23)Schneider Children's Medical Center of Israel- Sackler Faculty of Medicine- Tel-Aviv University, Institute of Gastroenterology- Nutrition and Liver Diseases-- Israel, Petach Tikva, Israel;(24)Meyer Children’s Hospital- University of Florence, Department NEUROFARBA- Gastroenterology and Nutrition Unit, Florence, Italy;(25)Sapienza University of Rome - Umberto I Hospital, Pediatric and Gastroenterology Unit, Rome, Italy;(26)Shaare Zedek Medical Center- The Hebrew University of Jerusalem, Juliet Keidan Institute of Pediatric Gastroenterology Hepatology and Nutrition, Jerusalem, Israel;
Background
Very early-onset inflammatory bowel disease (VEOIBD) is diagnosed before the age of 6 years while infantile IBD occurs before the age of 2 years. We aimed to assess disease characteristics and long-term outcomes in these populations.
Methods
We conducted a retrospective longitudinal cohort study in 21 pediatric centers worldwide. Patients diagnosed with VEOIBD between the years 2008-2018 with at least 2 years of follow-up were included.
Results
The cohort included 243 patients (52% males), with median follow-up of 5.8 (IQR 3.2-8.4) years. Median age at diagnosis was 3.3 (IQR 1.8-4.5) years, with 69 (28%) diagnosed before the age of 2 years. Disease was classified as Crohn’s disease (CD), ulcerative colitis (UC) and IBD-unclassified (IBDU) in 30%, 59% and 11%, respectively. In patients with UC or IBDU, 75% presented with pancolitis. In patients with CD, 62% presented with isolated colonic disease and 32% with ileo-colonic disease, while 19% had perianal involvement. Genetic testing was performed in 96 (40%) patients [40 (58%) <2 years, 56 (32%) 2-6 years, p=0.001], with monogenic diagnosis identified in 23% (33% and 16%, respectively, p=0.08). The most common findings were mutations in IL10-receptor (5 cases, 23%). Stricturing or penetrating disease was observed in 9 cases (4%).
First induction therapies were corticosteroids, 5-aminosalicylic acid (5ASA) and nutritional therapy in 53%, 30% and 11%, respectively. Corticosteroids were more common as first induction in infantile vs. non-infantile IBD (64% vs. 49% respectively, p=0.003). Maintenance therapies included deep immune-suppression (mainly biologics and corticosteroids) in 51%, immunomodulators in 27%, and non-immunosuppressive agents (5-ASA, nutritional therapy and antibiotics) in 22% of patients, with no significant differences between age groups.
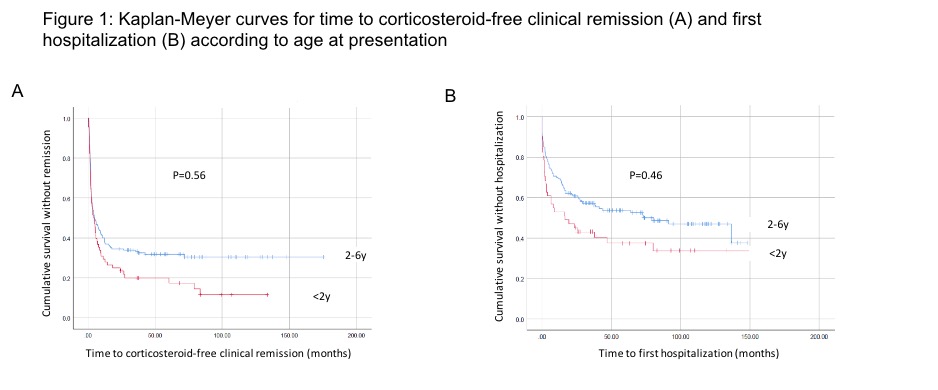
Compared to patients diagnosed after 2 years of age, patients with infantile IBD presented with higher rates of IBDU, lower levels of hemoglobin and albumin and higher levels of CRP, lower weight (but not height) z-scores, had lower rates of response to first induction therapy and shorter time to hospitalization during follow-up (p<0.05 for all).
Colectomy was performed in 11% and diversion surgery in 4% of the cohort, with no significant differences between age groups. No malignancies and nor deaths were observed. At end of follow-up, 85% of patients were in corticosteroid free clinical remission.
Conclusion
Patients with VEOIBD, including infantile IBD, have fair long-term outcome with low rates of complications and surgical interventions. Nevertheless, patients with infantile IBD demonstrated more severe clinical features at presentation and a lower response to induction therapy.


