N02 The importance of the multidisciplinary team (MDT) and its impact on quality of life and medication adherence in patients with Inflammatory Bowel Disease
Herrerias, G.(1);Barros, J.R.(2);Lopes, M.A.(1);Saad-Hossne, R.(3);Baima, J.P.(4);Sassaki, L.Y.(4);
(1)São Paulo State University Unesp- Medical School- Botucatu, medical clinic department, Botucatu, Brazil;(2)Federal University of Rio de Janeiro- Macae- Brazil, Nursing Institute, Macaé/RJ, Brazil;(3)São Paulo State University Unesp- Medical School- Botucatu/SP, Department of surgery and orthopedics, Botucatu/SP, Brazil;(4)São Paulo State University Unesp- Medical School- Botucatu/SP, Department of Clinical Medicine, Botucatu/SP, Brazil;
Background
IBD is a chronic immune-mediated disease that requires continuous patient care. The frequent contact and the good relationship with the multidisciplinary team (MDT) are essential for improving quality of life (QoL) and medication adherence aiming at treatment success. The aim of the study was to assess the importance of MDT in the view of patients with IBD and its impact on QoL and in medication adherence.
Methods
A cross-sectional study was carried out, including 114 patients from an IBD reference center in Brazil. The relevance of MDT was assessed through a questionnaire that included the importance of physicians, nurses, nutritionists and psychologists in the patient care. QoL was assessed by IBDQ. Treatment adherence and knowledge about the disease were assessed using the Morisky and CCKNOW questionnaires, respectively.
Results
: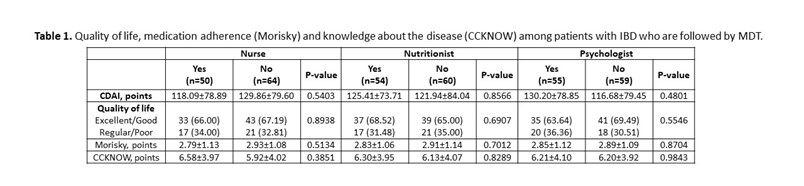 In total, 69 (60.53%) patients with CD and 45 (39.47%) patients with UC were included. The mean age was 39.16 (±13.50) years and 58.77% were female. The disease duration was 9.88 (±7.35) years. Presence of comorbidities was observed in 52.63% patients. About 57 (82.61%) patients with CD use biological therapy, with a statistical difference (p <0.0001) when compared to patients with UC (37.78%). The gastroenterologist was considered very important by 91.23% of patients, coloproctologist by 62.07% of patients, nurse by 65.05% of patients, nutritionist by 50% of patients and psychologist by 47.25% of patients. In the analysis of QoL, 24 (21.05%) patients had excellent QoL, 52 (45.61%) had good QoL, 29 (25.44%) had regular QoL and 9 (7.89%) had poor QoL, with no difference between patients who followed with nurses or other MDT professionals (Table 1). Medication adherence was low in 58.88% of patients. Knowledge about the disease was low (6.21 ± 3.99 points), being higher among patients with CD (p = 0.01). Patients identify the doctor as the main provider of care for their health, but about 10% leave with doubts from their appointments. 10% of patients think that more care with the nurse is necessary and less than 10% of patients are clarified by the nurse about QoL, ostomies, fecal incontinence, disease activity, biological therapy and sexuality.
In total, 69 (60.53%) patients with CD and 45 (39.47%) patients with UC were included. The mean age was 39.16 (±13.50) years and 58.77% were female. The disease duration was 9.88 (±7.35) years. Presence of comorbidities was observed in 52.63% patients. About 57 (82.61%) patients with CD use biological therapy, with a statistical difference (p <0.0001) when compared to patients with UC (37.78%). The gastroenterologist was considered very important by 91.23% of patients, coloproctologist by 62.07% of patients, nurse by 65.05% of patients, nutritionist by 50% of patients and psychologist by 47.25% of patients. In the analysis of QoL, 24 (21.05%) patients had excellent QoL, 52 (45.61%) had good QoL, 29 (25.44%) had regular QoL and 9 (7.89%) had poor QoL, with no difference between patients who followed with nurses or other MDT professionals (Table 1). Medication adherence was low in 58.88% of patients. Knowledge about the disease was low (6.21 ± 3.99 points), being higher among patients with CD (p = 0.01). Patients identify the doctor as the main provider of care for their health, but about 10% leave with doubts from their appointments. 10% of patients think that more care with the nurse is necessary and less than 10% of patients are clarified by the nurse about QoL, ostomies, fecal incontinence, disease activity, biological therapy and sexuality.
Conclusion
Patients considered doctors as the most important professionals in their care. Although the service has a multidisciplinary team, not all patients had the opportunity to consult with all professionals, mainly do the Covid pandemic in 2020 and 2021. The lack of contact with the entire team, especially with the nurse, may have contributed to low medication adherence and low knowledge of the disease, impacting disease control and QoL.


