N03 Introducing video consultations as part of an IBD tight monitoring care pathway: interim results of the INTERACTION project
Hoefkens, E.(1)*;Lembrechts, N.(1);Bossuyt, P.(1);Pouillon, L.(1);
(1)Imelda General Hospital, Gastroenterology, Bonheiden, Belgium;
Background
IBD requires tight monitoring of disease activity. E-health applications are associated with improved clinical outcomes and have a positive impact on healthcare costs. INTERACTION (telemedIciNe as parT of an intEgRAted IBD Care paThway @Imelda bONheiden) is a pilot project exploring the feasibility of implementation of teleconsultation in an existing tight monitoring care pathway and potential (dis)advantages for patients, health-care workers and quality-of-care.
Methods
INTERACTION is an ongoing, single-centre feasibility project including patients with moderate-to-severe IBD (UC/CD) treated with immunomodulators, subcutaneous biotherapy or oral small molecules since February 2022. Eligibility criteria include (i) stable treatment and remission, based on physician global assessment, patient-reported outcomes (UC: SCCAI<3; CD: PRO-2 ≤11), and faecal calprotectin (<250 µg/g) or endoscopy (UC: MES ≤1; CD: SES-CD ≤5), and (ii) digital access.. Participants agreed to embark in an adapted care pathway implementing video consultations with the treating physician alternating with in-person consultations. PRO’s and biomarkers were collected on dedicated time points (Figure 1). Patients’ expectations were questioned at the start of the pathway. Outcomes included patients’ experiences (assessed with the adapted Telehealth Usability Questionnaire), socio-economic impact, and clinical evolution (IBD-related flares or hospitalizations).
Results
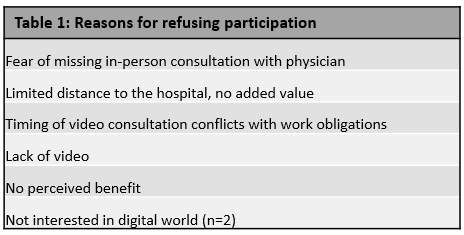
At the moment of interim analysis (Oct 24th 2022), 37/44 (84%) invited patients wanted to participate. The majority expected that teleconsultations could be equal to in-person consultations (86%) and lead to an increased access to healthcare (92%) and time gain (97%). Seven patients refused participation for various reasons (Table 1). Four patients were screen failures due to lack of remission. Ultimately, 33 patients (baseline characteristics: Table 2) underwent a total of 67 consultations. The majority (92%) experienced the video consultations as (strongly) satisfactory (Figure 2). Patients’ time savings with video consultation compared to an in-person consultation varied between 0-30’ (16%); 30-60’ (36%), 60-120’ (36%) and more than 120’ (12%). The majority (92%) avoided a round trip to the hospital of at least 10 km. Forty percent averted absenteeism. One patient experienced an IBD flare without the need for hospitalisation during the median follow-up of 3 (IQR 3-5.5) months .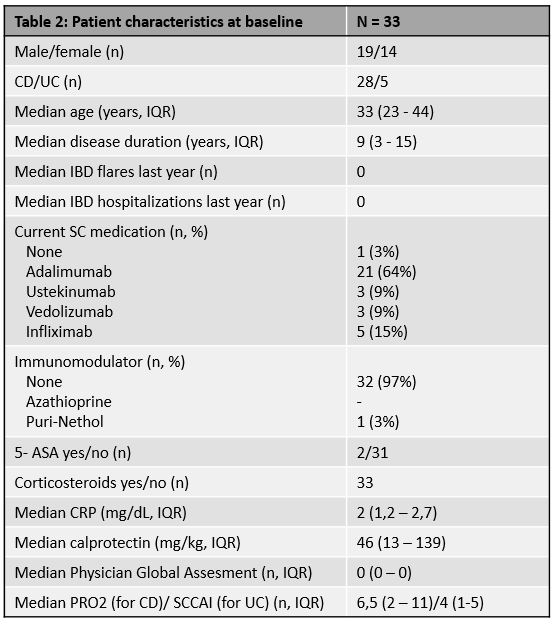

Conclusion
Implementing video consultations in the IBD care pathway of the ongoing INTERACTION project seems feasible, well-received and safe in patients with IBD in stable remission. In a second phase, video consultations led by an advanced IBD-nurse warrant further exploration.