OP02 Impact of therapeutic strategies on intestinal resection rate in paediatric inflammatory bowel diseases: A population-based cohort study over a 24-year period (1988–2011)
D. Ley1, A. Leroyer2, C. Dupont3, H. Sarter2, V. Bertrand4, C. Spyckerelle5, N. Guillon2, B. Pariente6, G. Savoye7, D. Turck1, C. Gower-Rousseau2, M. Fumery8, Epimad group
1Paediatric Gastroenterology Unit, Lille University Hospital and Lille University, Lille, France, 2Epidemiology and Public Health, Lille University Hospital and Lille University, Lille, France, 3Paediatric Unit, Caen University Hospital, Caen, France, 4Paediatric Unit, Havre Hospital, Havre, France, 5Paediatric Unit, Saint Vincent Hospital, Lille, France, 6Gastroenterology Unit, Lille University Hospital and Lille University, Lille, France, 7Gastroenterology Unit, Rouen University Hospital and Rouen University, Rouen, France, 8Gastroenterology Unit, Amiens University Hospital and Amiens University, Amiens, France
Background
Few data are available at the population level on the impact of the changes in therapeutic strategies over the last decades on inflammatory bowel diseases (IBD) long-term outcomes. We have evaluated the impact of immunosuppressants (IS) and anti-TNF introduction on intestinal resection rate, hospitalisation, and Crohn’s disease (CD) behaviour progression in a large population-based paediatric-onset IBD cohort.
Methods
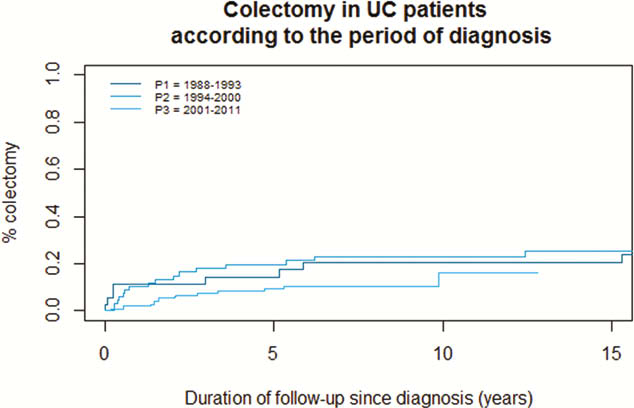
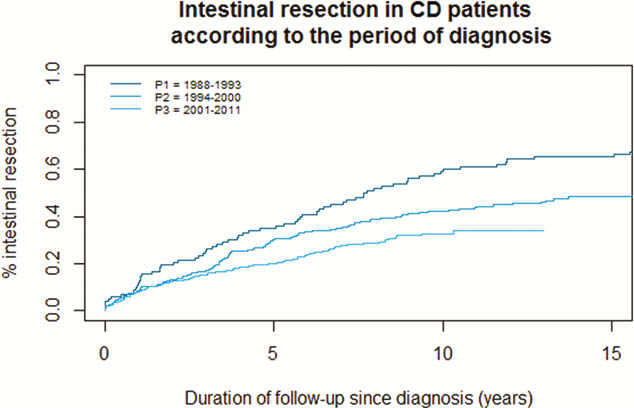
Paediatric-onset IBD (<17 years) were issued from a prospective population-based study in France between 1988 and 2011 and were retrospectively followed until 2013. Risks for intestinal resection, hospitalisation and complicated CD behaviour (stricturing or penetrating) were compared between three diagnostic periods: 1988–1993 (P1), 1994–2000 (P2) and 2001–2011 (P3) using Kaplan–Meier survival analyses.
Results
One thousand and sixty-one patients diagnosed with CD (
Conclusion
In parallel with the increased use of IS and anti-TNF agents, risk for intestinal resection within 5 years after diagnosis decreased in paediatric CD, whereas risks for flare-related hospitalisation and behaviour progression remained unchanged over a 24-year period.


