OP19 Gaps between ECCO quality standards of care and the real world: the E-QUALITY survey
Fiorino, G.(1)*;
(1)Vita e Salute University, Gastroenterology and Digestive Endoscopy, Milan, Italy;
Background
Recently, the European Crohn’s and Colitis Organisation (ECCO) Consensus on Quality-of-Care (QoC) Standards proposed essential criteria on the structure of units who manage patients with inflammatory bowel disease (IBD)1. The E-QUALITY taskforce investigated whether there is a gap between the given recommendations and the real-world structure of IBD units across ECCO-affiliated countries.
Methods
The E-QUALITY task force developed a web survey accessible to all institutions affiliated to ECCO across Europe. Each institution was invited by email to participate. Only one delegate per institution was requested to respond to the 48 questions listed in the web questionnaire. A descriptive analysis was done.
Results
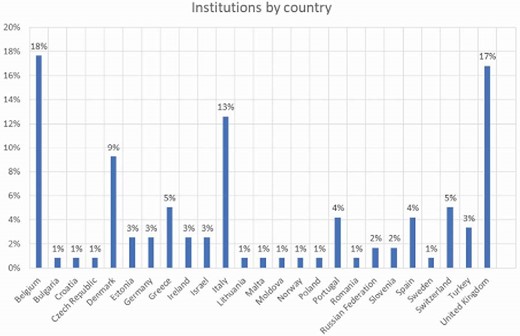
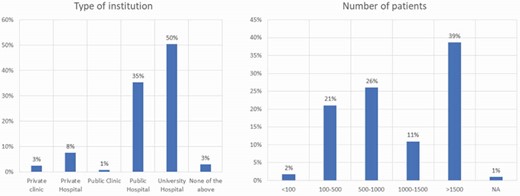
Data were collected from September 2022 to December 2022. One-hundred nineteen institutions from 24 countries responded (Figure 1). Characteristics of the institutions are shown in Figure 2. Overall, 80 (67%) institutions identified their hospital as an IBD Unit, 75 (63%) had identified IBD sub-specialists (4 on average per hospital), 66 (55%) had a dedicated IBD nurse, 69 (58%) had an IBD surgeon, and 92 (77%) had a referral pathway for complex IBD surgery. In 81 (68%) institutions there was a regular MDT discussion of IBD cases. The multidisciplinary team (MDT) included at least one pathologist in 80 (67%) institutions, a radiologist in 86 (72%), a dietitian in 69 (58%), and a stoma specialist in 79 (66%). In 107 (90%) institutions, timely access to another sub-specialist (i.e., dermatologist, rheumatologist) was provided. Paediatric-to-adult transition clinics were available in 66 (55%) institutions. In 77 (64%) institutions, departmental IBD management guidelines were reported however, only 56 (47%) developed and applied quality indicators. Almost all institutions (113, 95%) provide direct contact to patients, mainly by telephone and email, and 105 (88%) provide remote follow-up to their IBD patients. In 111 (93%) institutions, there were facilities to administer intravenous therapies, 103 (86%) had an integrated hospital emergency department, 107 (90%) had inpatient admission rights, and 86 (82%) defined a pathway for early recognition of flares. Collaboration with patients’ associations was present in 99 (83%) of institutions, and a patient database was available in 88 (74%). Lack of dedicated funds, protected time and shortage of personnel were regarded as the three main challenges to achieving and maintaining QoC.
Conclusion
Our survey has revealed that the structure of IBD units across Europe seems to be consistent with the ECCO standards, although some gaps still exist. ECCO will improve programs and initiatives to help institutions provide standard QoC across countries.
References: 1. Fiorino G, Lytras T, Younge L, et al. Quality of care standards in inflammatory bowel diseases: A european crohn's and colitis organisation [ecco] position paper. Journal of Crohn's & colitis 2020;14:1037-48.


