P013 The JAK-3 and TYK-2 / STAT pathways are activated in moderate to severe ulcerative colitis
M. Loza1, J.M. Brea1, C. Calviño-Suarez2, I. Baston-Rey2, R. Ferreiro-Iglesias2, J.E. Dominguez-Munoz2, M. Barreiro-de Acosta2
1BioFarma Research Group, CIMUS Research Center and IDIS Health Research Institute, Department of Pharmacology, Santiago de Compostela, Spain, 2Department of Gastroenterology, IBD Unit, University Hospital Santiago De Compostela CHUS, Santiago De Compostela, Spain
Background
Ulcerative colitis (UC) is a chronic, progressive and disabling disease with a complex pathology of unknown aetiology influenced by genetic, environmental and microbiota factors that lead to an immunological and inflammatory response in the colon. Janus Activated Kinase (JAK) family plays a key role in modulating the adaptive and innate inflammatory response. The JAK/STAT pathway involvement in UC has been demonstrated in both animal models and human studies. Thus, overexpressed JAK-3 has been detected in the intestine of patients with UC, suggesting a key role in their pathophysiology and the inhibition of TYK-2 in animal models resulted in an improvement of the disease, which would explain its implication in the inflammatory process. We hypothesise here that there could be an activation of JAK-3 and TYK-2 signalling pathways in UC patients. Thus, we aimed to detect the activation of both signalling pathways by means of western-blot studies in UC patient samples
Methods
A prospective, observational single-centre study was designed. Inclusion criteria were adult patients with endoscopic active UC (more than Mayo-0) confirmed in a programmed colonoscopy. All patients signed informed consent. Samples were obtained from overstock of routine biopsies in the more severe segment affected of the large bowel. Tissues were homogenised and processed in order to obtain cell lysates by employing RIPA buffer and ultrasounds. The degree of activation of the JAK-3 and TYK-2 pathways was measured by detecting the phosphorylation of both targets as well as of STAT1, STAT3, STAT4, STAT5 and STAT6 through western blot by employing specific antibodies for total and phosphorylated proteins.
Results
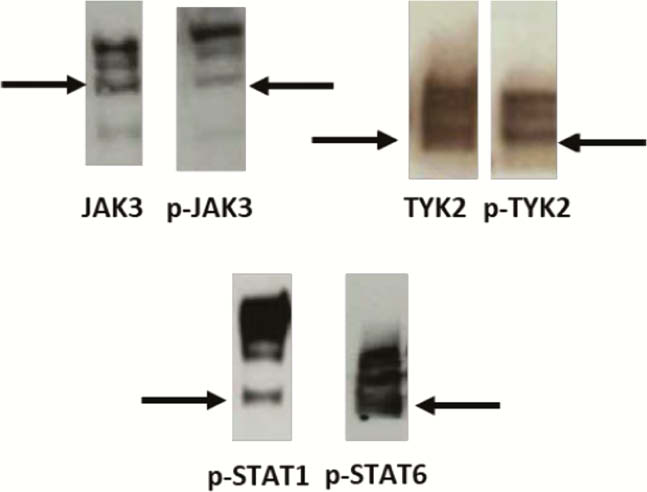
19 UC patients were consecutively included. Mean age was 46 years old. 53% were female, 47% were extensive colitis (E3) and 53% left-side colitis (E2). Regarding endoscopic activity, 26% had Mayo-1, 53% Mayo-2, and 21% Mayo-3. Immunoreactive bands for both phosphorylated JAK-3 and TYK-2 were detected in the biopsies from UC patients, evidencing that colonic inflammation leads to an activation of both targets. The study of STATs phosphorylation showed immunoreactive bands for phosphorylated forms of STAT1, STAT3, STAT4, STAT5 and STAT6 confirming the activation of both signalling-pathways in these patients (Figure 1).
Conclusion
The developed translational workflows involving basic/clinical research confirm the activation of both JAK-3 and TYK-2-dependent signalling pathways in UC patients, validating both kinases as targets for treating UC. The developed methodology allows studying the target engagement for future JAK-3/ TYK-2 inhibitors employed in clinical trials.


