P030 Dynamics of intestinal inflammation and microbial dysbiosis in pregnant women with IBD and their infants
L. Tarassishin PhD1, E. Kim2, C. Eisele1, A. Barre3, A. Thjømøe4, E. Mørk4, M. Dubinsky5, J. Stone6, N. Nair1, A. Debebe1, K. Hawkins1, A. Rendon1, J. Sabino7, J. Torres8, J.F. Colombel9, I. Peter1, J. Hu1
1Department of Genetics and Genomic Sciences, Icahn School of Medicine at Mount Sinai, New York, USA, 2School of Medicine, Department of Internal Medicine, Kyungpook National University- Daegu, Korea- Republic of, 3Gastroenterology Division, Cochin University Hospital, Paris, France, 4Calpro AS, Calpro AS, Lysaker, Norway, 5Division of Pediatric Gastroenterology and Hepatology, Icahn School of Medicine at Mount Sinai, New York, USA, 6Department of Obstetrics, Gynecology and Reproductive Sciences, Icahn School of Medicine at Mount Sinai, New York, USA, 7Department of Gastroenterology, University Hospital of Leuven, Leuven, Belgium, 8Gastroenterology Division, Hospital Beatriz Angelo, Loures, Portugal, 9Division of Gastroenterology, Department of Medicine, Icahn School of Medicine at Mount Sinai, New York, USA
Background
IBD often affects women during their reproductive years; however, the effect of pregnancy on disease course remains poorly understood. We aimed to assess intestinal inflammation in IBD patients compared with controls as measured by faecal calprotectin (FC). We also investigated whether maternal IBD diagnosis was associated with altered FC in the offspring and if there were particular bacterial taxa that correlated with FC levels.
Methods
Pregnant women with or without IBD and their infants were prospectively enrolled in the MECONIUM study during 2015–2018 years. FC levels at each trimester of pregnancy and in babies throughout the first 3 years of life were measured using a quantitative enzyme immunoassay (CALPRO AS, Norway). Multivariate regression analysis was applied to investigate FC levels. Stool microbiota composition in the maternal and baby stool was assessed using 16s rRNA sequencing.
Results
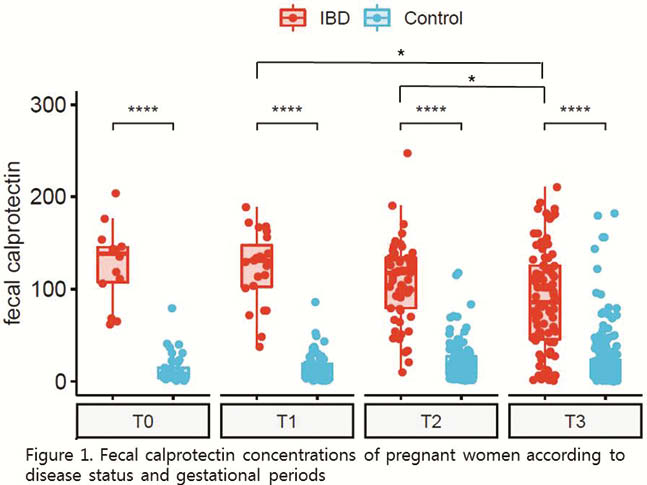
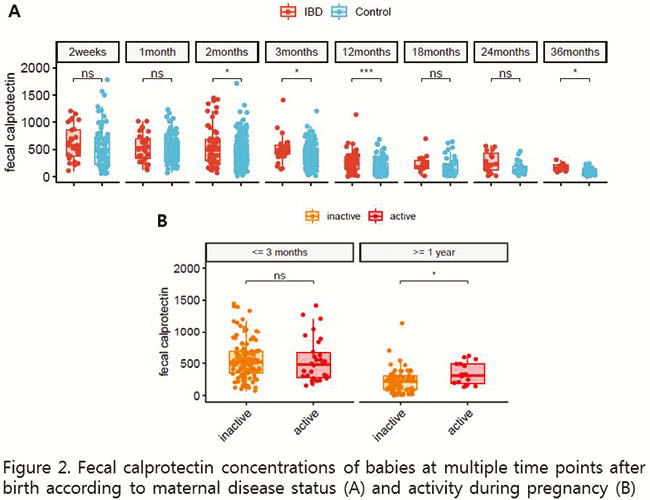
617 faecal samples from 342 mothers (91 IBD, 251 control) and 1005 faecal samples from 288 infants (born to 76 mothers with and 212 without IBD) were analysed. FC levels in pregnant women with IBD were significantly higher than in control pregnant women regardless of IBD type (Crohn’s disease vs. ulcerative colitis). In IBD mothers FC levels showed a decline during pregnancy (µg/g, median (interquartile range); first trimester 130.8 (102.3–147.3) vs. third trimester 85.9 (44.5–125.4),
Conclusion
FC levels in IBD patients decreased throughout pregnancy. Maternal IBD, lower microbiome diversity and the abundance of certain microbial genera were associated with higher FC in the offspring up to 3 years of life. These findings suggest a potential favourable impact of pregnancy on IBD activity and highlight a possible effect of IBD during pregnancy on the intestinal inflammation in offspring, which could be mediated through altered microbiome.


