P046 Vitamin D decreases PDIA3 and prevents the enhanced migration of fibroblasts from stricturing Crohn’s disease
L. Gisbert-Ferrandiz1, J. Cosín-Roger2, S. Coll1, C. Bauset1, D. Ortiz-Masiá3, F. Navarro-Vicente4, R. Alos5, S. Calatayud1, M.D. Barrachina1
1Department of Pharmacology, University Of Valencia, Valencia, Spain, 2FISABIO, Hospital Dr.Peset, Valencia, Spain, 3Department of Medicine, University Of Valencia, Valencia, Spain, 4Hospital Manises, Surgery, Valencia, Spain, 5Hospital La Fe, Surgery, Valencia, Spain
Background
Fibrosis is a common complication in Crohn’s disease (CD) patients and fibroblasts play an important role in the fibrogenic process. Low vitamin D (VD) levels and a defective VD-signalling pathway have been reported in CD. VD signals through both vitamin D receptor (VDR) and protein disulfide-isomerase A3 (PDIA3) and we have previously demonstrated that VDR protein levels are reduced in fibroblasts isolated from CD patients and that VD increased VDR expression in these cells (A-2080; ECCO 2019). We aim to analyse here the effect of VD on both PDIA3 protein levels and migration in CD fibroblasts.
Methods
We used intestinal fibroblasts isolated from surgical resections of the damaged mucosa of CD patients with stricturing behaviour (B2). Control fibroblasts were obtained from the non-damaged intestine of patients with colorectal cancer. Fibroblasts were treated with VD (100 nM) or its vehicle for 24 h and PDIA3 protein levels were measured by Western Blot. In the wound healing analysis, a single scraping was done in the centre of the fibroblasts monolayer and FBS-free medium was added to the cells, which allows us to determine the ability of fibroblasts to migrate and close the wound. Photos were taken at 0, 24 and 48 h. Results of wound healing were expressed as the percentage of the wound at each time point for the maximal wounded area (time 0, 100%). Statistical significance was measured by ANOVA or
Results
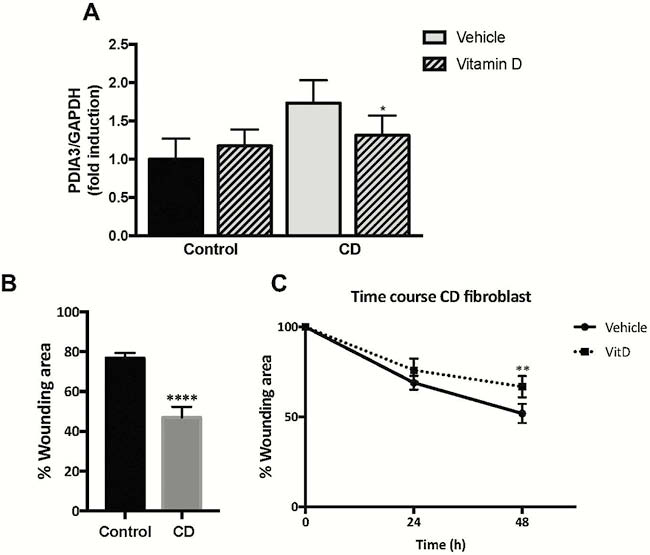
No significant differences in PDIA3 protein levels were detected between control and CD fibroblasts but VD significantly decreased PDIA3 expression in CD fibroblasts (Figure 1A). In the wound healing assay, we detected that CD-B2 fibroblasts migrate faster than control cells, resulting in a reduced wounding area, 48 h later (Figure 1B). Treatment of these CD-B2 cells with VD decreased their migration rate, and 48 h later cells exhibited a higher and significant wounding area than vehicle-treated cells (Figure 1C).
Conclusion
Vitamin D decreased PDIA3 expression and prevented the accelerated migration detected in intestinal fibroblasts from B2-CD patients which suggest an anti-fibrotic effect of VD mediated by a direct effect of this hormone on intestinal fibroblasts.


