P066 Azathioprine linked with impaired intestinal epithelial regeneration in Crohn’s disease
K. Borycka-Kiciak1, A. Pietrzak2,3, K. Ferenc4, P. Pietrzak4,5, L. Janaszek1, W. Tarnowski1, R. Zabielski4
1Orlowski Hospital, CPME, Department of General, Oncological and Gastrointestinal Surgery, Warsaw, Poland, 2Centre of Postgraduate Medical Education, Department of Gastroenterology, Hepatology and Clinical Oncology, Warsaw, Poland, 3Institute of Oncology, Department of Oncological Gastroenterology, Warsaw, Poland, 4Warsaw University of Life Sciences, Department of Large Animal Diseases with the Clinic, Faculty of Veterinary Medicine, Warsaw, Poland, 5Warsaw Agricultural University, Department of Physiological Sciences, Warsaw, Poland
Background
In patients operated due to active Crohn’s disease (CD), the negative effect of steroids and biologics on septic complications is known. Until now, azathioprine (AZA) is considered to be safe. The aim of our study was to assess the impact of AZA on intestinal epithelial cells damage in patients with active CD as a surrogate marker of healing.
Methods
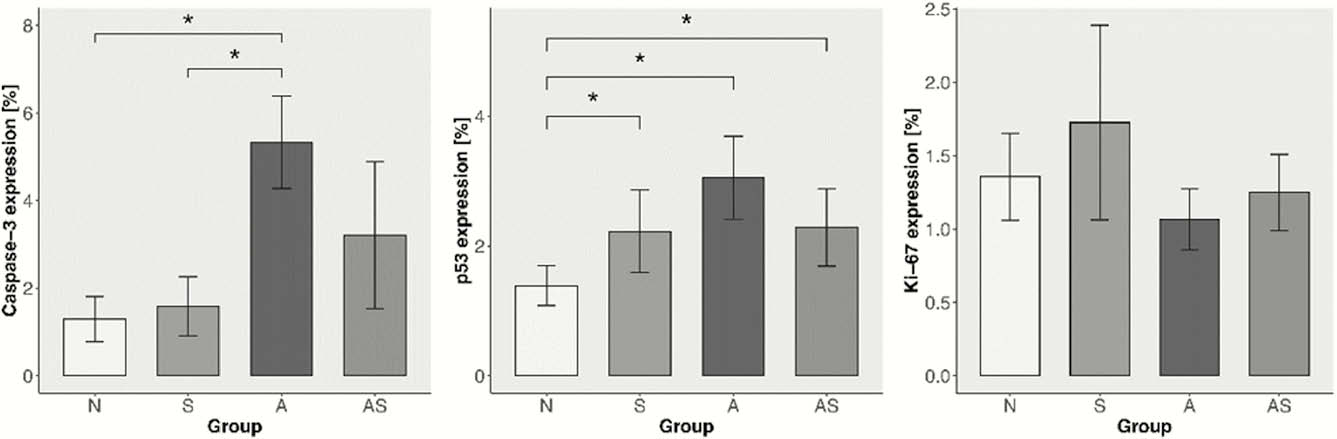
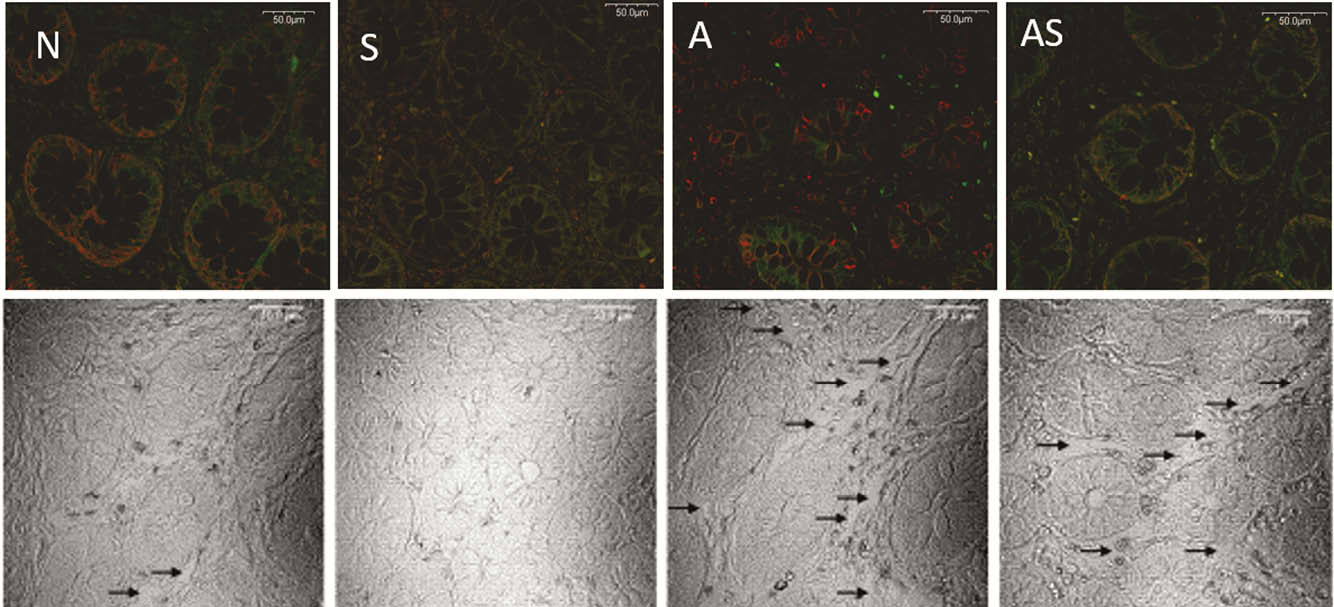
Intestinal specimens taken from macroscopically healthy surgical margins of all consecutive CD patients operated due to active isolated ileocecal disease during the study period (2014–2016) were evaluated. Expression of caspase-3, p-53 and Ki-67 as markers of cell apoptosis, DNA damage and proliferation were immunohistochemically tested and assessed using a confocal microscope and microimage for in-tissue-cytometry analysis. Western-blot analysis was performed for the evaluation of cellular integrity using ZO-1 and E-cadherin as a markers. 30-day clinical outcomes were assessed. The study was approved by the institutional Ethics Committee.
Results
From 61 operated due to active CD patients, 35 met the inclusion criteria. Patients were divided accordingly to preoperative treatment: treated with no immunomodulators (N-9 patients), on steroids (S-14 patients), on AZA (A-6 patients), and on combination therapy, AZA + steroids (AS-6 patients). There were no substantial differences between groups. We found statistically significant increase of apoptosis in A group compared with N (5.33 ± 1.05 vs. 1.29 ± 0.51,
Conclusion
We found that in epithelial cells of the small and large intestine of patients treated with AZA, apoptotic activity and DNA damage processes are increased when regeneration processes and mucosal integrity are significantly disturbed. These abnormalities of intestinal epithelial regeneration may be a surrogate marker of impaired mucosal healing.


