P076 Abdominal pain severity for IBD in remission correlates with genetic clustering and enzymatic activity of faeces-derived Candida albicans strains
Van Thiel, I.(1,2)*;Maasland, T.(3);van Wassenaer, E.(4);Hoekman, D.(5);Spooren, C.(6,7);Hakvoort, T.(1,8);Admiraal, I.(1,8);Theelen, B.(2);Levin, E.(3);Benninga, M.(5);Jonkers, D.(6,7);D'Haens, G.(4);Rosendahl, S.(9);Boekhout, T.(2,10);Hagen, F.(10,11,12);de Jonge, W.(1,4,13);van den Wijngaard, R.(1,4);
(1)AmsterdamUMC- loc. AMC, Tytgat Institute for Liver and Intestinal Research, Amsterdam, The Netherlands;(2)Westerdijk Fungal Biodiversity Institute, Yeast Research, Utrecht, The Netherlands;(3)Horaizon, Horaizon, Delft, The Netherlands;(4)AmsterdamUMC- loc. AMC, Department of Gastroenterology and Hepatology, Amsterdam, The Netherlands;(5)AmsterdamUMC- loc. AMC, Department of Pediatric Gastroenterology and Nutrition, Amsterdam, The Netherlands;(6)Maastricht University Medical Centers+, Department of Internal Medicine- Division Gastroenterology-Hepatology, Maastricht, The Netherlands;(7)Maastricht University, NUTRIM School of Nutrition and Translational Research in Metabolism, Maastricht, The Netherlands;(8)AmsterdamUMC- loc. AMC, Microbiota Center Amsterdam, Amsterdam, The Netherlands;(9)University of Copenhagen, Department of Biology- Section for Ecology & Evolution, Copenhagen, Denmark;(10)University of Amsterdam, Institute of Biodiversity and Ecosystem Dynamics IBED, Amsterdam, The Netherlands;(11)Westerdijk Fungal Biodiversity Institute, Medical Mycology Group, Utrecht, The Netherlands;(12)University Medical Center Utrecht, Medical Microbiology, Utrecht, The Netherlands;(13)University Hospital Bonn, Department of General- Visceral- Thoracic and Vascular Surgery, Bonn, Germany;
Background
Abdominal pain is a common occurrence for approximately 39% of patients with inflammatory bowel diseases in remission (quiescent IBD; qIBD). There is increasing evidence for a contributing role of the gastrointestinal fungal community (i.e., mycobiome) in relation to intestinal inflammation and irritable bowel syndrome (IBS). As such, abundance of Candida spp. and sub-species variation of Candida albicans were previously associated with IBD severity. In the current study, we aim to investigate mycobiome of patients with qIBD and qIBD with abdominal pain (qIBD–AP).
Methods
Patients with qIBD (defined as faecal calprotectin (FCP) ≤250 μg/g) with (n=91) or without (n=58) abdominal pain provided faecal samples. Abdominal pain was scored based on either the Irritable Bowel Syndrome Symptom Severity Scale (IBS–SSS) or Gastrointestinal Symptom Rating Score (GSRS) questionnaire. Faecal fungal communities were determined based on Internal Transcribed Spacer 1 (ITS1) sequencing. Cultivable yeasts from faecal samples were identified using Matrix Assisted Laser Deionization Time–of–Flight Mass Spectrometry. C. albicans strains (n=137 from 29 patients) were genotyped by ITS Sanger sequencing analysis and typing of seven microsatellite loci. Release of virulence-related enzymes (proteinase, phospholipase, lipase, esterase) by C. albicans was assessed through determination of precipitation zones on solid agar mediums containing enzyme-specific substrates.
Results
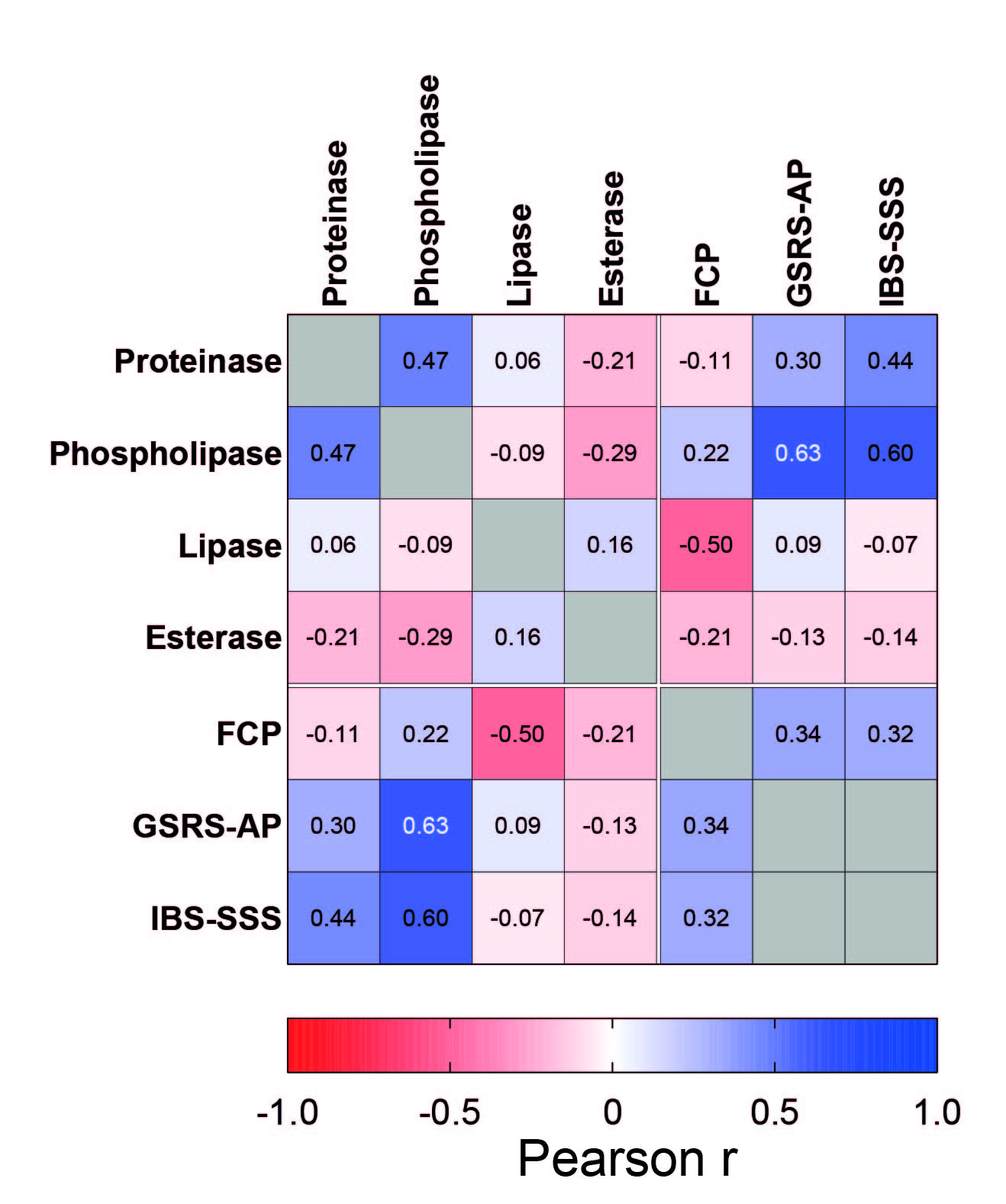
Descriptive mycobiota analysis revealed limited differences between compositions of qIBD and qIBD–AP patients, but a discriminative signature for abdominal pain was extracted using machine-based learning models. While ITS Sanger sequencing of faeces-derived C. albicans was insufficient to elucidate genetic variability, analysis of microsatellite loci revealed extensive variability and clustering into six clone clusters and a likely distinction between qIBD and qIBD-AP patients (Fig. 1). Phospholipase enzymatic activity of C. albicans strains correlated with GSRS–Abdominal Pain sub-score, as did proteinase activity with severity of abdominal pain according to the IBS–SSS (Fig. 2). Additionally, lipase activity inversely correlated with faecal calprotectin (Fig. 2).
Conclusion
The faecal gut mycobiome is associated with self–reported abdominal pain in patients with IBD in remission. This notion is based on both compositional and culture-dependent methods and specified clones of C. albicans may selectively contribute to abdominal pain for qIBD patients. This study opens further possibilities to investigate the role of faecal gut fungi in light of abdominal pain for qIBD-AP patients.


