P095 Initial disease course in a Belgian, prospective inception cohort of patients with inflammatory bowel disease: the PANTHER cohort
Verstockt, S.(1);Glorieus, E.(2);Ukunda, C.(3);Barbaraci, M.(3);Verstockt, B.(1,4);Sabino, J.(1,4);Ferrante, M.(1,4);Geldof, J.(2,5);De Vos, M.(2,5);Laukens, D.(5);Cleynen, I.(6);Vandermeulen, L.(3);Lobatón, T.(2,5);Vermeire, S.(1,4);
(1)KU Leuven, Department of Chronic Diseases- Metabolism and Ageing, Leuven, Belgium;(2)University Hospital of Ghent, Department of Gastroenterology, Ghent, Belgium;(3)Universitair Ziekenhuis Brussel UZ Brussel, Department of Gastroenterology, Brussels, Belgium;(4)University Hospitals Leuven, Department of Gastroenterology and Hepatology, Leuven, Belgium;(5)Ghent University, Department of Internal Medicine and Pediatrics, Ghent, Belgium;(6)KU Leuven, Department of Human Genetics, Leuven, Belgium
Background
Successful personalized treatment in inflammatory bowel disease (IBD) is critically dependent on identifying those patients at greater risk of a complicated disease course and who therefore may benefit from early advanced therapies. To this end, prospective inception cohorts integrating medical records with multi-omics data are needed. The Belgian Prognostic biobANk of paTients witH Early cRohn’s or colitis (PANTHER) was therefore initiated in 2015. We here present the initial disease course of this cohort.
Methods
The PANTHER cohort is an inception cohort of adult IBD patients from 3 Belgian, tertiary IBD referral centres. Patients are included within 3 months after diagnosis, are naïve for immunosuppressives and biologicals, and without previous IBD-related surgery. Clinical data are prospectively collected; and DNA, serum, feces and intestinal biopsies are taken at predefined time points. Patients are treated according to routine clinical management. Log-rank tests, and univariate and multivariate analyses were performed in R 3.6.2.
Results
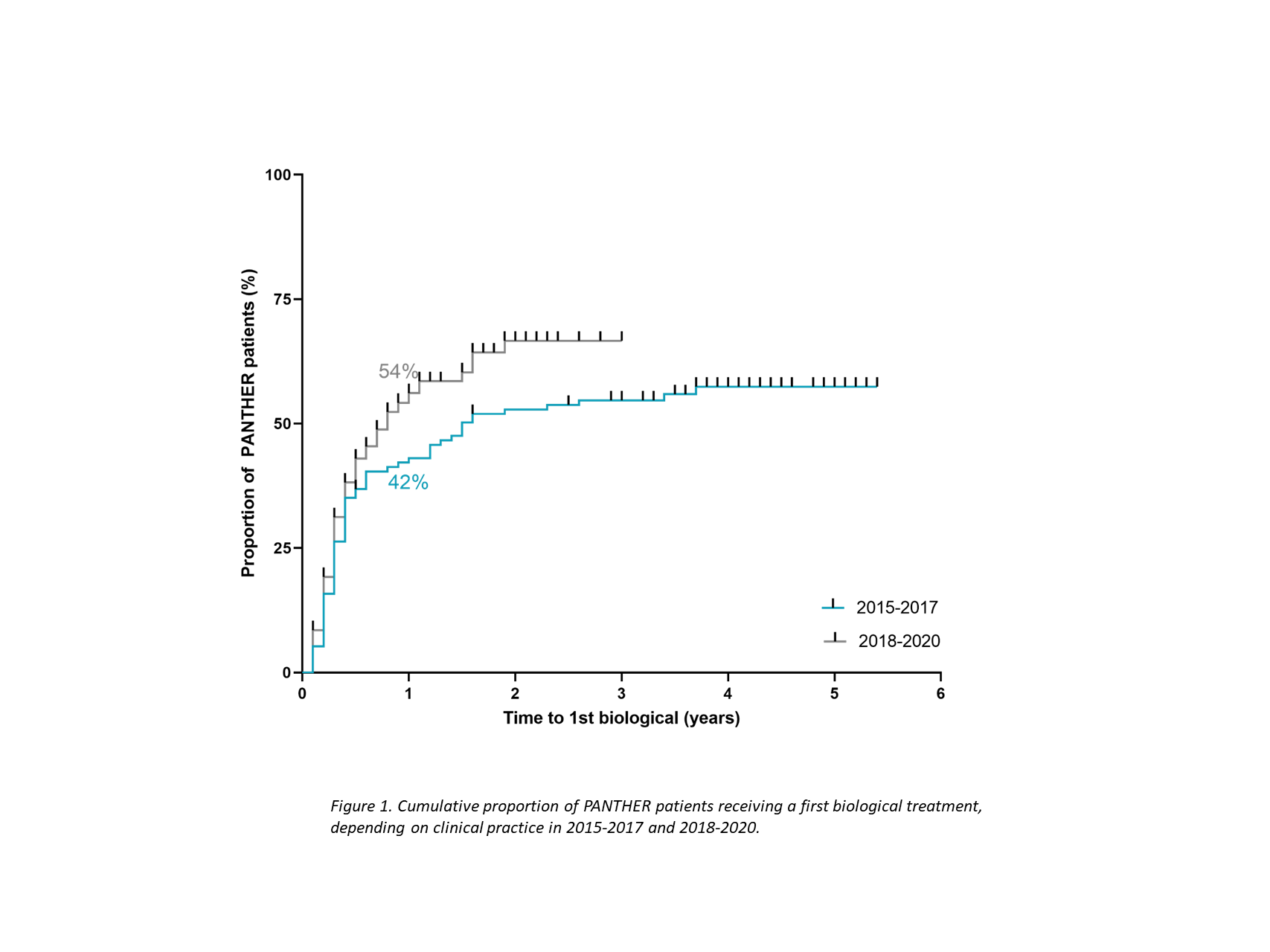
A total of 289 newly-diagnosed IBD patients were recruited (median [IQR] follow-up of 2.9 [1.4-4.2] years), of whom 161 (56%) had Crohn’s disease (CD), 122 (42%) had ulcerative colitis, and 6 (2%) had IBD type unclassified (Table 1). Thus far, 242 of these patients (83%) are minimally at 1-year follow-up. Twenty-two patients (9%) already needed surgery (n=5 for colectomy and n=17 for ileocecal or small bowel resection) and 124 patients (51%) received biological therapy within the 1st year after diagnosis. Time series analysis showed a clear trend for increase in biological use within the 1st year after diagnosis when comparing 2015-2017 (42%) to 2018-2020 (54%) (p=0.06) (Fig.1). Being exposed to a biological within the 1st year was associated with age (OR=0.98 [95%CI: 0.96-0.99]), CD diagnosis (OR=3.7 (95% CI: 2.2-6.3) and more recent diagnosis (2018-2020 as opposed to previous years) (OR=1.2 [95% CI: 1.2-3.4]). Within CD, perianal disease was the strongest driver for early biological use (OR=4.4 [95% CI: 1.8-12.8]). Early biological exposure led to clear trends in decreased surgery rates one year later (2/99 [2%]) as compared to non-exposed patients (8/108 [7%]) (p=0.07), while hospitalization rates significantly decreased (4% versus 12%, p=0.04).
Conclusion
In this Belgian inception cohort, an increase in early biological use is observed in recent years and is associated with reduced IBD-related surgery and -hospitalization.