P095 PD-1 expressing T cells in patients with different types of colitis
B. Roosenboom1, C. Horjus Talabur Horje1, C. Smids1, J.W. Leeuwis2, E. Van Koolwijk3, M. Groenen1, P. Wahab1, E. Van Lochem3
1Rijnstate Hospital, Department of Gastroenterology and Hepatology, Arnhem, The Netherlands, 2Rijnstate Hospital, Department of Pathology, Arnhem, The Netherlands, 3Rijnstate Hospital, Department of Microbiology and Immunology, Arnhem, The Netherlands
Background
Immunotherapy-related colitis is a frequent adverse event in patients with malignancies, treated with inhibitors targeting programmed death-1 (PD-1). This treatment leads to enhancement of lymphocyte activity, thereby generating antitumor T-cell activity. The role of PD-1+ T cells in the pathophysiology of different types of colitis is unclear. Therefore, we aimed to study the presence of PD-1+ T cells in inflammatory bowel disease (IBD), infectious colitis and healthy controls compared with anti-PD-1-related colitis.
Methods
We performed a prospective cohort study. Newly diagnosed patients with ulcerative colitis (UC,
Results
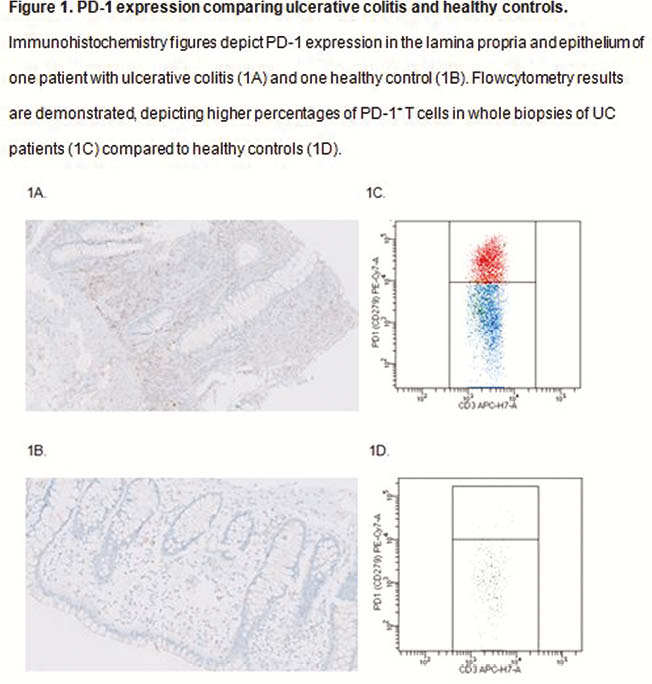
Using immunohistochemistry, PD-1 was not present on lymphocytes in the epithelium of patients with any type of colitis, nor in healthy controls. Of all lymphocytes in the lamina propria, % PD-1 expression was 40% in UC, 5% in infectious colitis, 3% in anti-PD-1-related colitis and 0% in healthy controls. PD-L1 was expressed on lymphocytes in the epithelium and lamina propria of UC patients (12.5% and 40%) and in infectious colitis (1% and 30%), whereas in anti-PD-1-related colitis (0% and 15%) and healthy controls (0% and 15%) no PD-L1+ lymphocytes were demonstrated in the epithelium. Flowcytometry showed higher percentages of PD-1+ T cells in biopsy specimens of UC patients (25.2% (IQR 17.9–35.6)) compared with all other groups; CD patients (13.5% (5.0–25.3),
Conclusion
In patients with different types of colitis and in healthy controls, PD-1 was only expressed on T cells in the lamina propria and not in the epithelium. The percentage of PD-1+ T cells was significantly higher in patients with UC compared with patients with CD or infectious colitis and healthy controls. As expected PD-1+ T cells were nearly absent in patients with anti-PD-1-related colitis.


