P117 Biomarkers of extracellular matrix remodelling are associated with intestinal fibrosis assessed by magnetic resonance enterography and accumulated intestinal damage (Lémann index): the IBSEN study
J. Mortensen1, A.K. Lunder2, T. Manon-Jensen1, M.A. Karsdal1, M.J. Nielsen1, D.J. Leeming1, J.R. Hov3, A. Negård2,4, J. Jahnsen4,5, B. Moum4,6, M. Vesterhus7,8,9,10, M.L. Høivik11, V.A. Kristensen11
1Nordic Bioscience A/S, Department of Biomarkers and Research, Herlev, Denmark, 2Akershus University Hospital, Department of Radiology, Lørenskog, Norway, 3University of Oslo, Department of Transplantation Medicine, Oslo, Norway, 4University of Oslo, Institute of Clinical Medicine, Oslo, Norway, 5Akershus University Hospital, Department of Gastroenterology, Lørenskog, Norway, 6University Hospital Oslo, Department of Gastroenterology, Oslo, Norway, 7Oslo University Hospital Rikshospitalet, Norwegian PSC Research Center, Oslo, Norway, 8Haraldsplass Deaconess Hospital, Department of Medicine, Bergen, Norway, 9University of Bergen, Department of Clinical Science, Bergen, Norway, 10Oslo University Hospital Rikshospitalet, Department of Transplantation Medicine, Oslo, Norway, 11Oslo University Hospital, Department of Gastroenterology, Oslo, Norway
Background
Magnetic resonance enterography (MRE) has become an important tool in the diagnosis and follow-up of Crohn’s disease (CD). MRE findings are used in the calculation of the Lémann index (LI), a score that quantifies accumulated bowel damage. However, calculating the score is demanding; thus, serum biomarkers reflecting tissue damage and fibrosis are warranted for monitoring purposes. Increased extracellular matrix (ECM) remodelling and collagen tissue deposition is the result of accumulated bowel damage, eventually leading to intestinal fibrosis; particularly, the basement membrane and interstitial matrix are affected. We aimed to investigate ECM serum biomarkers of type III collagen formation (PRO-C3), type IV collagen degradation (C4M), degradation of citrullinated vimentin (VICM) and their association with LI and the degree of bowel wall fibrosis assessed by contrast-enhanced MRE in CD patients.
Methods
Serum from CD patients was analysed (
Results
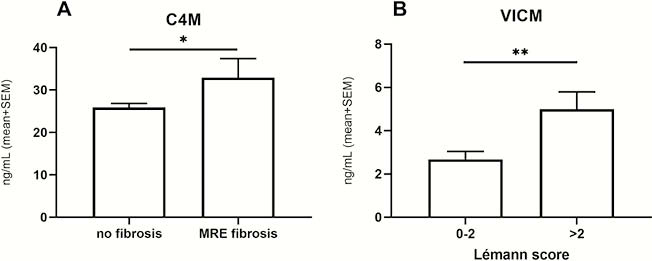
Serum levels of C4M were elevated in patients with confirmed fibrosis by contrast MRE compared with patients without fibrosis (
Conclusion
Our results indicate that the accumulated intestinal damage and the bowel wall fibrosis in CD are associated with elevated serum levels of VICM and C4M, respectively. Thus, serological biomarkers of basement membrane degradation and inflammation may be a useful tool to monitor intestinal tissue damage and fibrosis development.


