P122 External validation of the Picasso Histological Remission Index (PHRI) to assess endoscopic and histological remission and predict long-term outcome in Ulcerative Colitis: A multicentre prospective study.
ParigiMD, T.L.(1)*;Cannatelli, R.(2);Nardone, O.M.(3);Zammarchi, I.(4);Shivaji, U.(1);Furfaro, F.(5);Zardo, D.(6);Spaggiari, P.(7);Del Sordo, R.(8);Setti, O.(9);Majumder, S.(1);Smith, S.C.L.(1);Ghosh, S.(10);Danese, S.(5);Armuzzi, A.(11);Villanacci, V.(9);Iacucci, M.(1);
(1)University of Birmingham, Institute of Immunology and Immunotherapy, Birmingham, United Kingdom;(2)ASST Fatebenefratelli Sacco, Gastroenterology Unit, Milan, Italy;(3)University of Naples Federico II, Gastroenterology- Department of public health, Naples, Italy;(4)ASST-Spedali Civili Brescia, Gastroenterology Unit, Brescia, Italy;(5)IRCCS Ospedale San Raffaele, Department of Gastroenterology and Digestive Endoscopy, Milan, Italy;(6)University Hospitals Birmingham NHS Foundation Trust, Department of Histopathology, Birmingham, United Kingdom;(7)IRCCS Humanitas Research Hospital, Pathology Unit, Milan, Italy;(8)Medical School- University of Perugia, Department of Medicine and Surgery- Section of Anatomic Pathology and Histology, Perugia, Italy;(9)ASST-Spedali Civili Brescia, Institute of Pathology, Brescia, Italy;(10)University College of Cork, APC Microbiome Ireland- College of Medicine and Health, Cork, Ireland;(11)IRCSS Humanitas Research Hospital, IBD Center- Department of Gastroenterology, Milan, Italy;
Background
The PICaSSO Histological remission Index (PHRI) is a simple histological index for assessing ulcerative colitis (UC) based only on the presence or absence of neutrophils in the lamina propria, superficial and cryptal epithelium (Table 1), which can be implemented in artificial intelligence (AI) systems.1 We aimed to externally validate its correlation with endoscopy and its prognostic value.
Methods
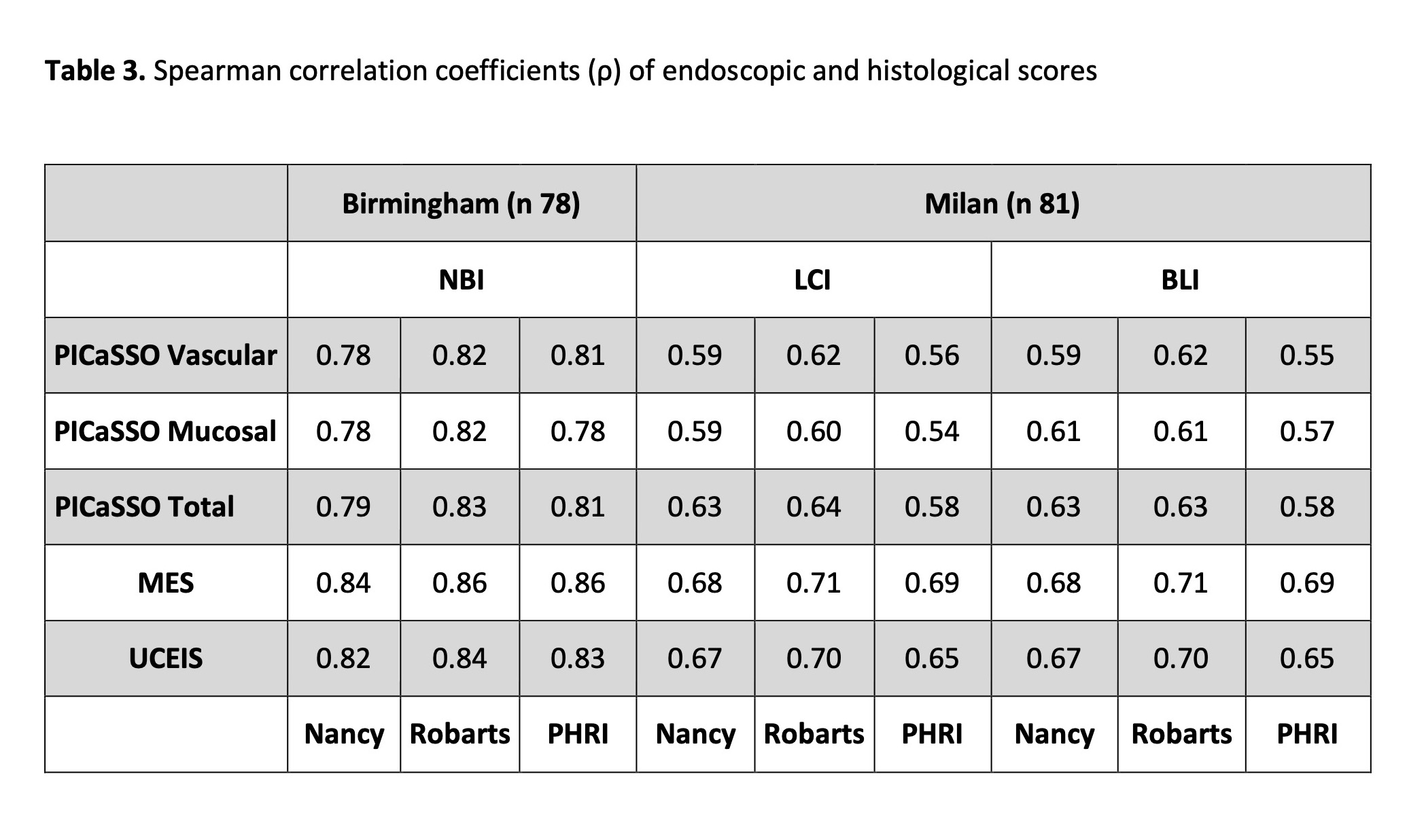
Patients with UC underwent colonoscopy in Birmingham, UK using white light+NBI, and in Milan, Italy, using white light+BLI/LCI. Participants were followed up for 2 years and occurrence of major adverse outcomes (UC-related hospitalization, UC treatment change/optimization, need for steroids, and colectomy) were recorded. We measured the correlation (Spearman coefficient) between histological scores (PHRI, Nancy [NHI] and Robarts [RHI]) and endoscopic scores (Mayo Endoscopic Score [MES]; Ulcerative Colitis Severity Endoscopic Index of Severity [UCEIS], and Paddington International virtual ChromoendoScopy ScOre [PICaSSO]). Vice versa, ROC curves were plotted for endoscopic scores to assess histological remission. Outcome analysis at 24 months was performed according to the Cochran-Mantel-Haenszel method, Kaplan-Meier curves were plotted and hazard ratios were calculated.
Results
159 patients were enrolled, 79 in the NBI cohort and 81 in the BLI/LCI cohort. Demographic characteristics are detailed in Table 2.
PHRI correlated with all endoscopic scores regardless of the type of virtual chromoendoscopy. In particular, in the NBI cohort correlations were 0.86, 0.83 and 0.81 for MES, UCEIS and PICaSSO, respectively; and 0.69, 0.65 and 0.58 in the BLI/LCI cohort. Correlation with endoscopy was also similar between PHRI, Nancy and Robarts. Table 3.
The area under the ROC curve (AUROC) in the NBI cohort for MES, UCEIS and PICaSSO were 0.95 (95% CI 0.91-1.00), 0.95 (95% CI 0.90-1.00), and 0.93 (95% CI 0.87-0.99), respectively. Similarly, in the BLI/LCI cohort AUROCs were 0.86 (95% CI 0.78-0.94), 0.88 (95% CI 0.81-0.95) and 0.85 (95% CI 0.77-0.94).
At survival analysis (Figure 1), Kaplan Meier curves appeared similar, and the hazard ratio (HR) between patients histologically active or in remission in the NBI cohort were 3.11 (95% CI 1.47-6.57), 2.93 (95% CI 1.36-6.32) and 2.19 (95% CI 1.07-4.53) for PHRI, RHI and NHI, respectively; and 2.82 (95% CI 1.54-5.15), 2.82 (95% CI 1.54-5.16) and 2.82 (95% CI 1.54-5.15) in the BLI/LCI cohort.


Conclusion
We confirmed PHRI’s correlation with endoscopy, its similar performance with RHI and NHI, and its prognostic value in two independent cohorts. Neutrophil-only assessment of UC is a simple reliable alternative to current histological scores and a useful tool for AI systems.
Reference
1 Gui X. et al. Gut, 2022


