P124 Clock gene expression levels can differentially distinguish between ulcerative colitis and Crohn’s disease
Y. Weintraub1, S. Cohen1, N. Chapnik2, A. Yerushalmy-Feler1, A. Ben-Tov1, I. Dotan3, R. Tauman4, O. Froy2
1Sourasky Medical Center, Tel Aviv-Israel, Pediatric Gastroenterology, Tel Aviv, Israel, 2The Hebrew University, Institute of Biochemistry, Food Science and Nutrition, the Robert H Smith Faculty of Agriculture- Food and Environment, Rehovot, Israel, 3Rabin Medical Center, Division of Gastroenterology, Petah Tikva, Israel, 4Sourasky Medical Center, Tel Aviv-Israel, Sleep Disorders Center, Tel Aviv, Israel
Background
Pathophysiological mechanisms active in inflammatory bowel disease (IBD), such as mucosal barrier repair, innate and adaptive immune responses, intestinal motility and gut microbiome, all exhibit diurnal variations. Chronic disruption of the molecular clock augments inflammatory response. We have shown that newly diagnosed, naïve to treatment, young IBD patients showed reduced clock gene expression in both inflamed and non-inflamed intestinal tissues and in peripheral White blood cells (WBCs). This reduction correlated with disease activity1. Our aim in the current study was to determine whether certain clock genes correlate with disease activity scores or inflammatory markers in Crohn’s disease (CD) vs. ulcerative colitis (UC).
Methods
Fourteen CD and 11 UC patients, 8–22 years old, were recruited. Patients were evaluated upon diagnosis and during medical treatment. Disease activity scores, C-reactive protein (CRP) and faecal calprotectin (Fcal) levels were measured and WBC were analysed for clock gene (
Results
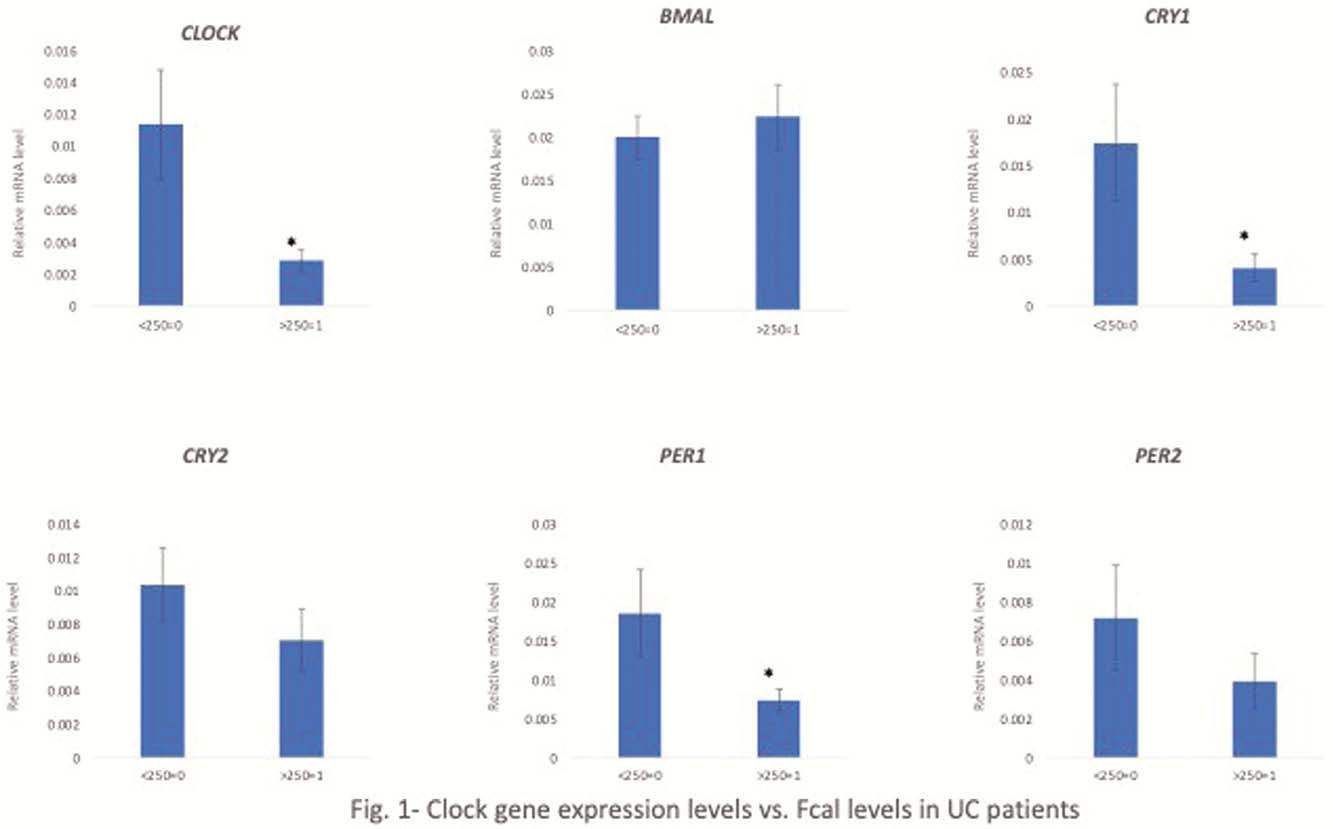
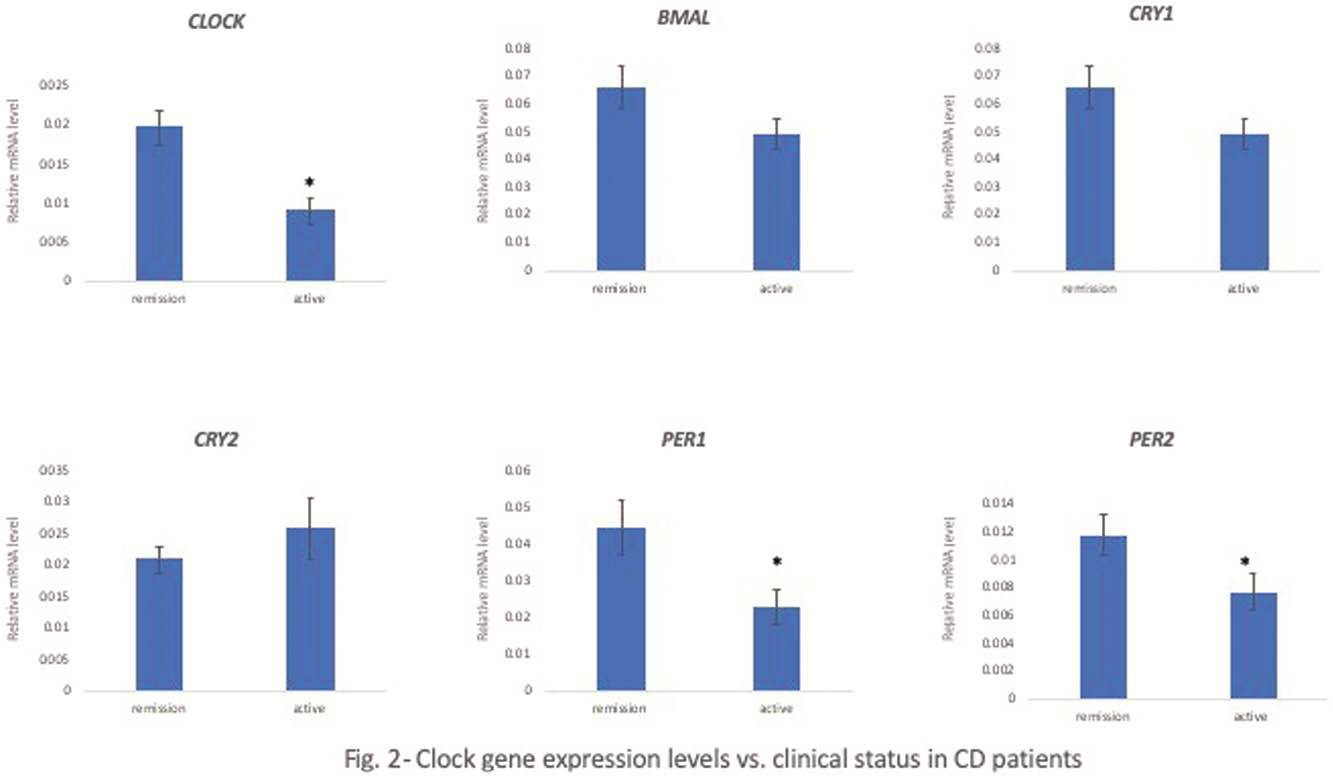
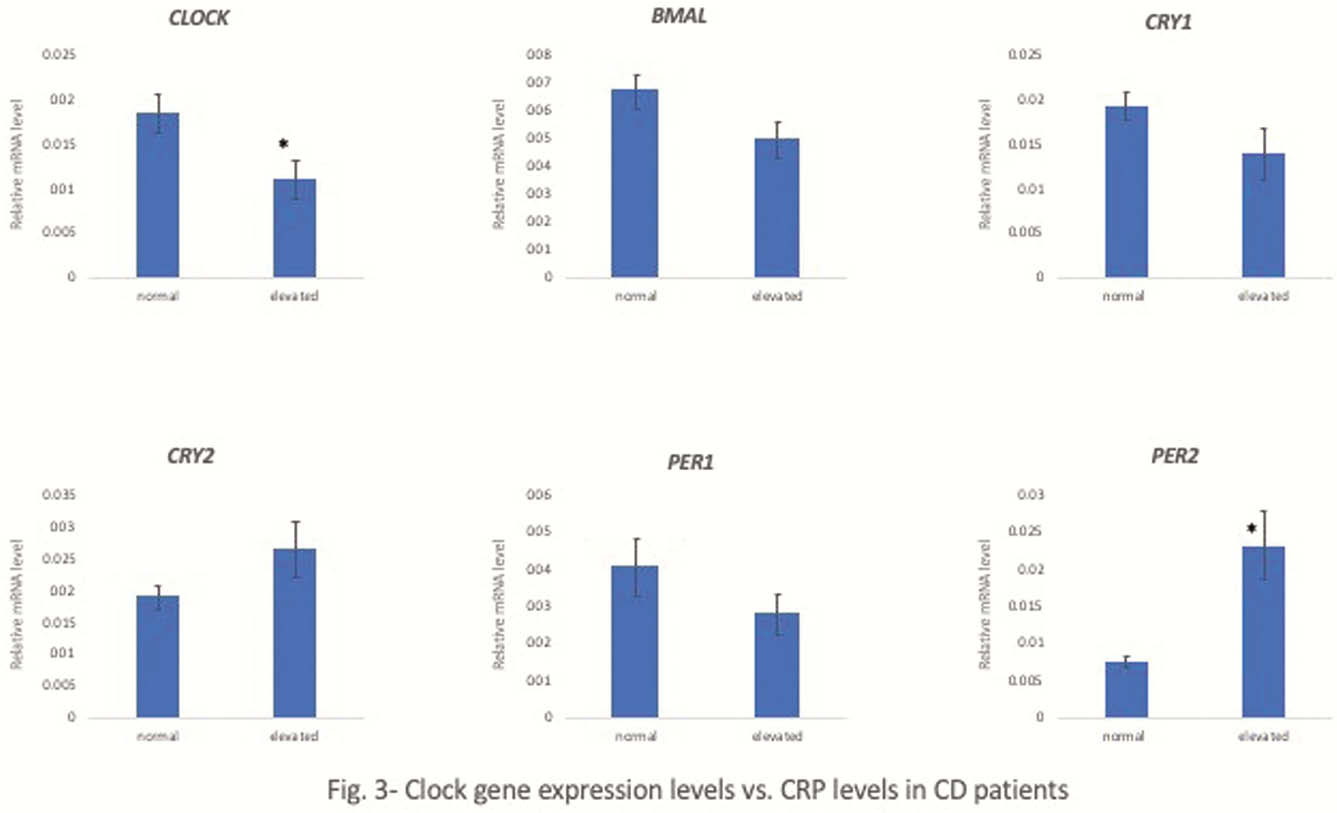
In UC,
Conclusion
Altered levels of certain clock genes were demonstrated in young CD and UC patients in relapse vs. remission and correlated with Fcal in UC patients and clinical status as well as CRP levels in CD patients.
Weintraub Y et. al, Clin Gastroenterol Hepatol. 2019 Apr


