P131 Is stress associated with subclinical inflammation in Ulcerative Colitis? A population-based cross-sectional cohort study in southeastern Sweden
Borghede, M.(1)*;Marsal, J.(2);Faresjö, T.(3);Hjortswang, H.(1);
(1)Linköping University, Department of Gastroenterology, Linköping, Sweden;(2)Lund University, Department of Clinical Sciences, Lund, Sweden;(3)Linköping University, Department of Clinical and Experimental Medicine, Linköping, Sweden;
Background
Ulcerative colitis (UC) is an immune-mediated chronic inflammatory bowel disease with a relapsing course. Whether perceived stress affects the disease activity remains debated. This study aimed to investigate if clinical and subclinical disease activity, perceived stress, and hair cortisol concentration (HCC) are associated.
Methods
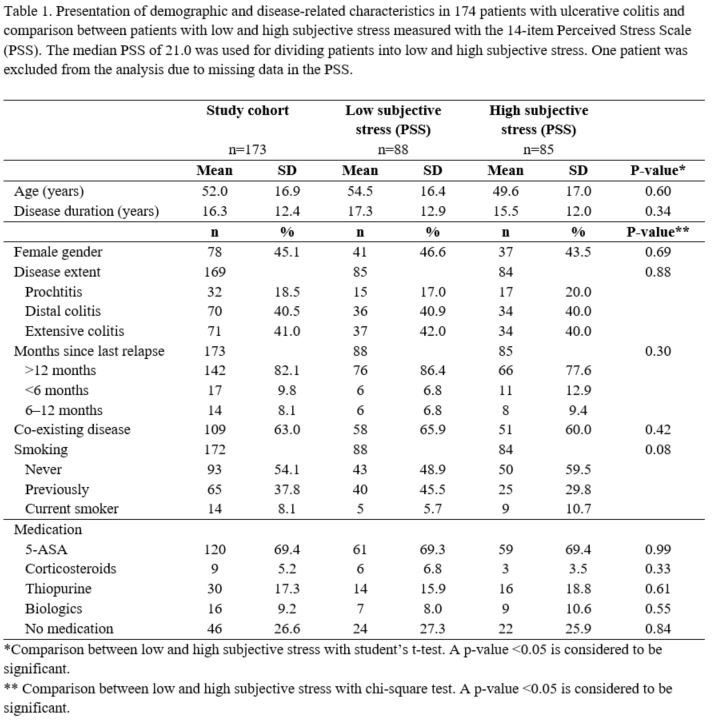
We performed a population-based cross-sectional cohort study with 200 randomly selected adult patients with UC living in the catchment area of Linköping University Hospital in southeastern Sweden. Demographic and disease-related data, bowel symptoms registration, the 14-item Perceived Stress Scale (PSS), the Short Health Scale (SHS), the Inflammatory Bowel Disease Questionnaire (IBDQ), fecal calprotectin (FC), CRP, and hair samples for hair cortisol concentration (HCC) were gathered. HCC has proven a reliable marker of long-term stress, with one centimeter of scalp hair accounting for approximately 4–6 weeks of stress level. A PRO2 score was calculated. Clinical remission was defined as a PRO2 score of zero.
Results
174 patients participated in the study (45.1% females). The median age was 52.0 years (IQR 40.0–65.0) and the median disease duration was 13.0 years (IQR 6.0–24.0). The median PSS score was 21.0 (IQR 16.0–27.0). 124 patients had a PRO2 score of zero. Patients in clinical remission had a significantly lower PSS score (median 21.0 (IQR 15.0–27.0)) compared to those with PRO2≥1 (median 24.0 (IQR 17.5–27.5)) (p<0.01). Patients experiencing more perceived stress (PSS score>21.0) had an impaired quality of life as measured with the SHS (p<0.01) and the IBDQ (p<0.01) compared with patients with lower PSS scores. The median FC was 43.1 µg/g, CRP 1.5 mg/l and HCC 24.7 pg/mg. HCC was lower in patients with clinically active disease (median 21.9 pg/mg) compared with patients in clinical remission (median 26.0 pg/mg) (p<0.05). No significant differences in FC, CRP or HCC were detected comparing patients with high versus low PSS scores. Neither was a correlation between HCC and FC or CRP observed.
Conclusion
Bowel symptoms contribute to the feeling of being stressed. Perceived stress is associated with impaired QoL. Among patients in clinical remission, no association between subclinical inflammation (FC), and perceived stress or long-term stress (HCC) was observed. The issue of whether perceived stress may cause or augment intestinal inflammation, or vice versa, requires further investigation.