P140 Costs of home-monitoring by telemedicine versus standard care management of Inflammatory Bowel Disease – a Danish register-based five-year follow-up study
Al-Sheikh, M.(1)*;Olsen, J.(2);Spangaard, M.(2);Egedesø, P.(2);Peters-Lehm, C.(1);Fjordside, E.(1);Bennedsen, M.(1);Burisch, J.(1);Munkholm, P.(1);
(1)North Zealand University Hospital, Department of Gastroenterology, Greater Copenhagen, Denmark;(2)Incentive, health economic, Holte, Denmark;
Background
The increasing incidence of Inflammatory bowel diseases (IBD) with subsequent increasing use of costly biological treatments such as well as the need for tight control of IBD places a significant economic direct and indirect cost burden on health care systems. Thus, eCare Constant-Care APP, home-monitoring of Patient Reported Outcome (PROs-SCCAI/HB-I, quality of life QoL, Disability index WEB-DI) and calprotectin (POCT-Point of Care Test) was introduced at North Zealand Hospital (NOH) in Denmark in 2015.
The aim of this study was to assess long-term cost effectiveness of remote telemedicine services (eCare) compared to standard care (sCare) for IBD patients during 5 years follow-up.
Methods
A retrospective register-based study was carried out among patients with ulcerative colitis (UC) or Crohn’s disease (CD) continuously included in the telemedicine service Constant Care (CC) in 2015-2020. Direct and indirect healthcare costs over a 5-year period were obtained from Danish registers and compared to a control group of IBD patients from all five regions in Denmark who were 1:5 matched on year of birth, gender, education, income, disease, use of biologics, duration of disease and Charlson Comorbidity index. The IBD patients (cases and controls) were identified in the National Patient Register (NPR) via registered ICD-10 diagnosis codes. Direct and indirect costs were estimated on a yearly basis from two years before inclusion in CC (i.e., the index year) and five years after using a linear regression model.
Results
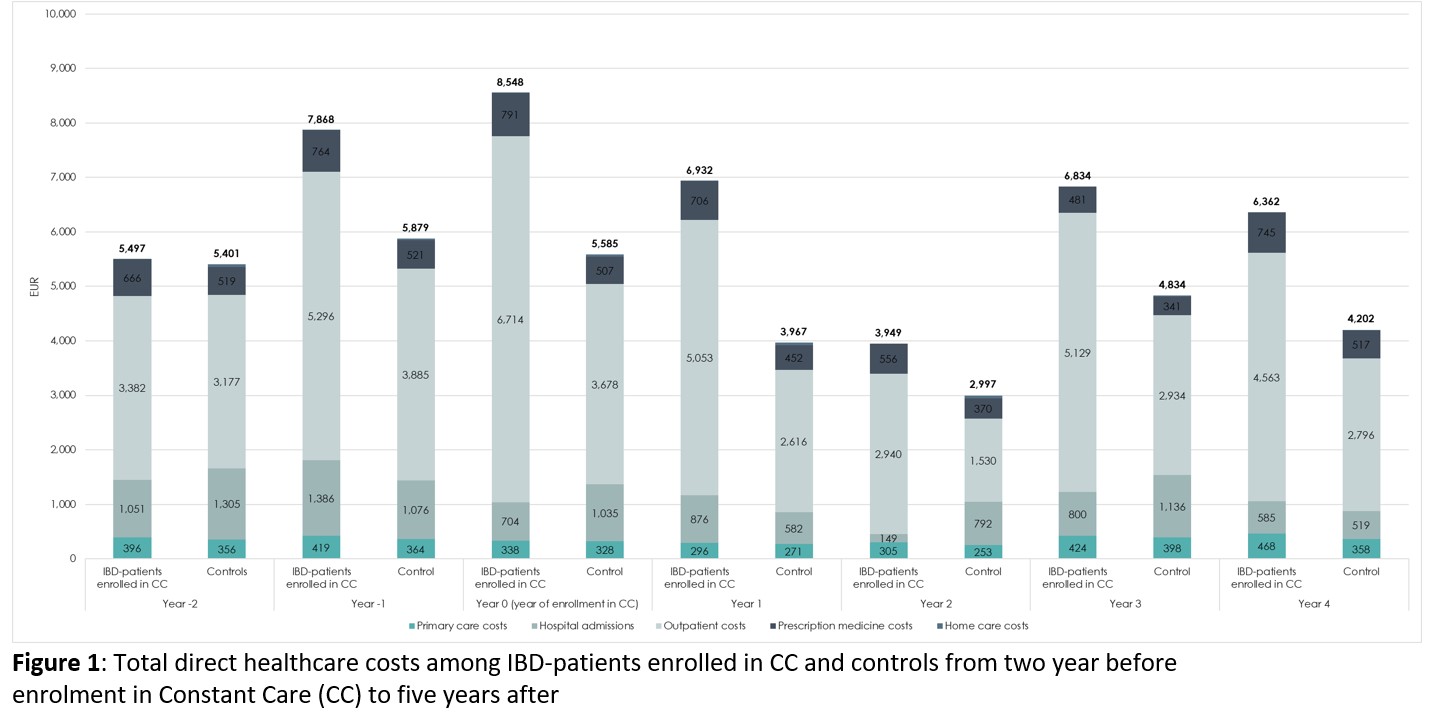
A total of 572 IBD patients were included in the study. Average annual costs of IBD-related outpatient visits were significantly (P<.005) higher among patients enrolled in CC compared to controls before and after index date whereas costs of hospital admissions were non-significant (ns). However, a slight decrease was observed in year 2 and 5 from index year (ns). The total direct costs were higher among CC patients compared to controls in the year prior to enrollment in CC and the five years after (Figure 1) primarily driven by the costs of outpatient visits.
Significantly (P<.05) fewer CC patients were on early retirement compared to controls and CC patients received less public transfer payments compared to controls (ns).
Conclusion
Telemedicine care was associated with higher cost than standard care. One potential confounder is inefficient out-patient registration in NRP which highlights the need for continuous validation of clinical registration approaches in Denmark. A prospective RCT is warranted in future.