P153 IBD patients’ treatment preferences are heterogeneous, but largely affected by the avoidance of abdominal pain and side effects (P-POWER IBD study)
Louis, E.(1);Siegel, C.A.(2);James, B.(3);Heidenreich, S.(4);Krucien, N.(4);Ghosh, S.(5);
(1)CHU de Liège et Université de Liè, Gastroenterology, Liège, Belgium;(2)Dartmouth-Hitchcock Medical Center, Gastroenterology and Hepatology, Lebanon NH, United States;(3)Abbvie, Gastroenterology, Mettawa, United States;(4)Evidera Ltd., Patient-centered Research, London, United Kingdom;(5)College of Medical and Dental Sciences University of Birmingham, Institute of Translational Medicine, Birmingham, United Kingdom
Background
Multiple treatments are approved for inflammatory bowel disease (IBD), each offering unique attribute profiles. Therapeutic targets historically included clinical and endoscopic outcomes, but updated guidelines1 also include absence of disability and restoration of quality of life (QoL). Optimising QoL requires understanding patient priorities and considering their preferences in treatment selection. This patient preference study (P-POWER IBD) quantified the tradeoffs patients would make between treatment attributes.
Methods
Adults with self-confirmed Crohn’s disease (CD) or ulcerative colitis (UC) who were receiving IBD treatment took part in an online cross-sectional survey. In a discrete choice experiment (DCE), patients were asked to choose between hypothetical treatments described by six attributes: administration, risk of mild or moderate side effects, risk of serious infections, and impact on abdominal pain, bowel urgency and fatigue. Attributes were selected based on foundational qualitative research and literature review.2 Qualitative and quantitative pilots were used to pre-test the DCE. Relative Attribute Importance (RAI) scores and maximum acceptable risk (MAR) of mild-to-moderate side effects were estimated from a mixed multinomial logit model.
Results
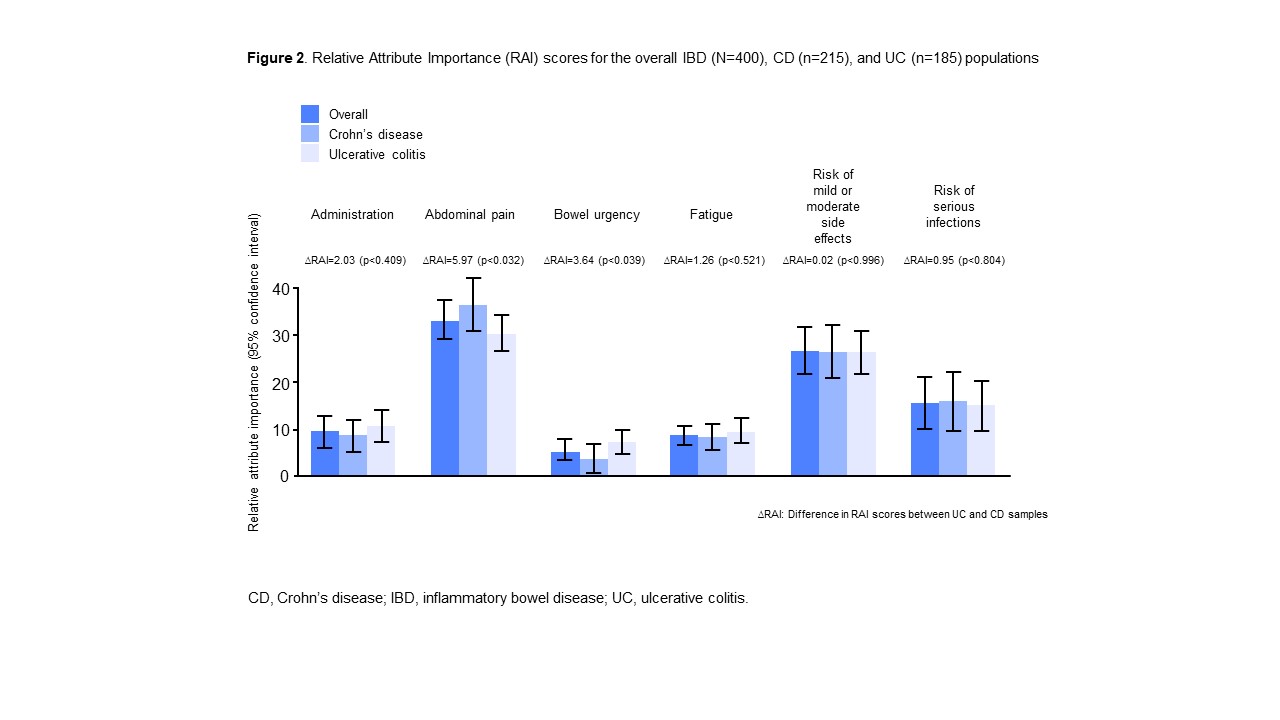
A total of 400 patients (CD: 54%; UC: 46%; female: 38%; mean age: 41 years [range: 18–78]) were recruited. All attributes significantly affected treatment preferences with preference heterogeneity observed (Figure 1). While all attributes were important, their relative importance differed (Figure 2). Avoiding abdominal pain was most important (RAI 33%) followed by the risk of mild or moderate side effects (RAI 27%), risk of serious infections (RAI 16%), treatment administration (RAI 10%), fatigue (RAI 9%), and bowel urgency (RAI 6%). CD patients placed greater importance on abdominal pain (p<0.05) than UC patients and UC patients greater importance on bowel urgency than CD patients (p<0.05). MAR indicated the increased risks of side effects patients would accept to improve other attributes (Figure 3). Notably, to reduce abdominal pain from severe to moderate, patients would accept an additional 19% risk of mild or moderate side effects and 31% if the pain was reduced to mild.
Conclusion
Patients with IBD had strong preferences that varied greatly and were willing and able to make tradeoffs between various important treatment attributes, in particular abdominal pain. Individual preferences should be considered in clinical practice as they may impact long-term targets and QoL.
References
1. Turner D et al. Gastroenterology 2020 https://doi.org/10.1053/j.gastro.2020.12.031
2. Louis E et al. Patient 2020;13:317–25