P159 Patients with Inflammatory Bowel Disease Present with Lower Trabecular Bone Scores
Yarur, A.(1);Alexandra, B.(1);Beniwal-Patel, P.(1);Stein, D.(1);Nunez, L.(1);Berens, B.(1);Shaina, S.(1);Parakkal , D.(2);Shaker, J.(3);Jenna, S.(3);
(1)Medical College of Wisconsin, Department of Gastroenterology, Milwaukee, United States;(2)Washington University, Medicine, St. Louis, United States;(3)Medical College of Wisconsin, Department of Endocrinology, Milwaukee, United States
Background
Patients with inflammatory bowel diseases (IBD) have lower bone mineral density (BMD). However, BMD does not reflect bone micro-structure/geometry, nor indicates the intrinsic properties of bone tissue. The trabecular bone score (TBS) delivers an indirect measurement of bone microarchitecture and predicts fracture risk independent of bone density. The aim of this study was to assess if patients with IBD present with lower TBS vs a healthy control (HC) population and to identify variables associated with lower TBS.
Methods
This prospective cohort study included patients with active Crohn’s disease (CD) or ulcerative colitis (UC) and a matched HC group. Patients with ostomies, short gut or known endocrine co-morbidities associated with low BMD, patients with osteoporosis on pharmacologic therapy were excluded. L1-L4 TBS and BMD parameters were determined by dual-energy X-ray absorptiometry (DXA) using a GE Lunar iDXA scan and TBS iNsight™ and GE enCORE™. Other collected variables included demographics, disease phenotype, laboratories (25-OH vitamin D [25OHD] and parathyroid hormone levels [PTH]), disease activity (c-reactive protein [CRP], simple endoscopic score [SES-CD] in CD, and endoscopic Mayo score [EMS] in UC). IBD severity was stratified based on endoscopy: mild (EMS=1 in UC or SES-CD=3-6), moderate (EMS=2 or SES-CD=7-15) and severe (EMS=3 or SES-CD>15). The primary outcome was the L1-L4 TBS. Secondary outcomes were left total and neck femoral BMD and the L1-L4 region BMD.
Results
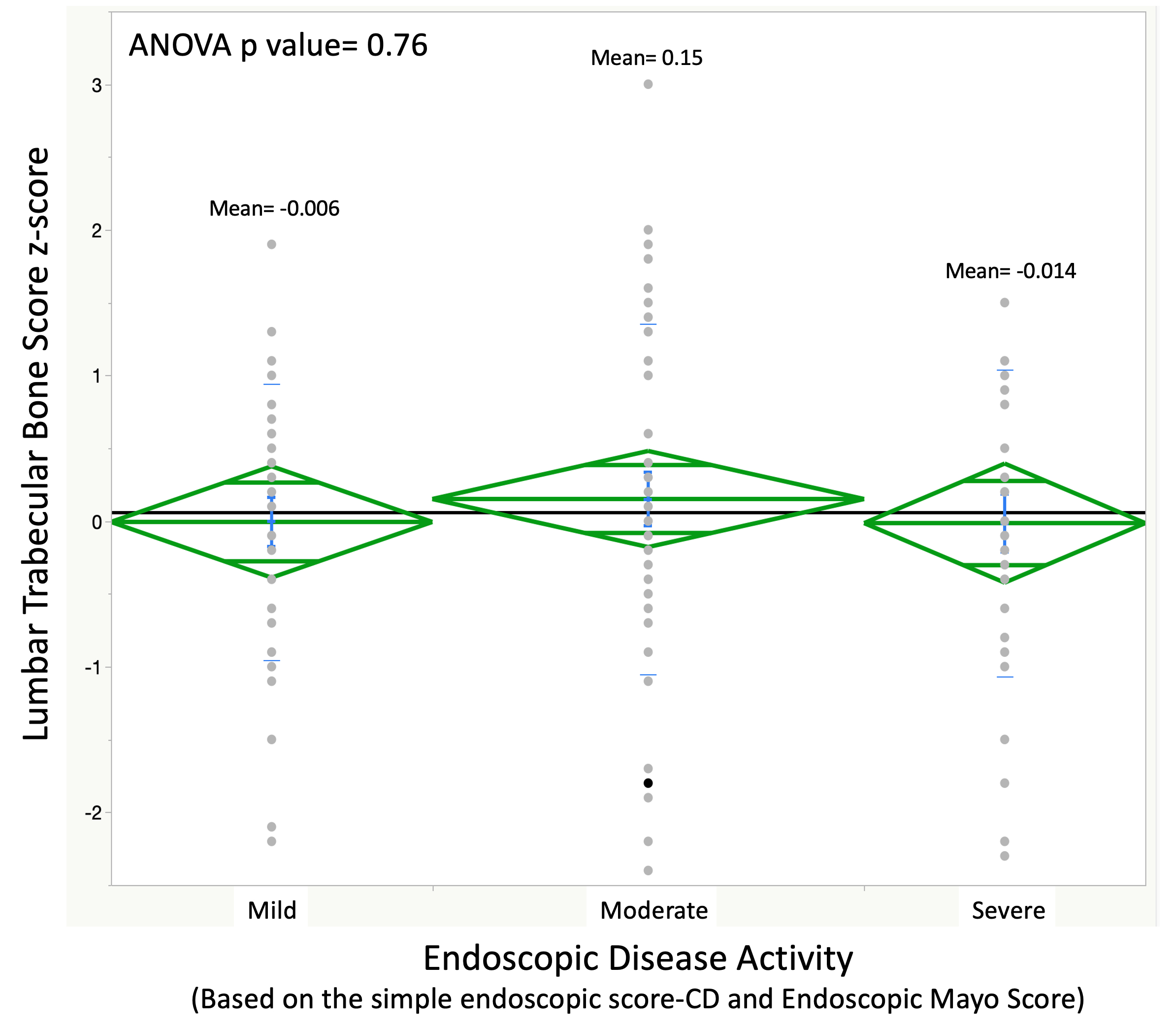
A total of 141 patients were included (115 IBD and 26 HC). Patients with IBD had significantly lower TBS, femoral and L1-L4 BMD and Z-Scores when compared to controls (Figure 1). Endoscopic disease activity was not associated with TBS (Figure 2) or total/neck femur and L1-L4 BMD and Z-scores (p>0.05 for all). When stratifying levels by 25OHD quartiles, patients with 25OHD ≥28 ng/mL (the highest 50th percentile of the study population) had significantly higher TBS Z-scores when compared to those with 25OHD ≤28 ng/mL (0.3 [-0.2 – 1.1] vs -0.1 [-1.1 – 0.5], p=0.002). No associations were seen between TBS Z-scores and use of steroids, gender, type of IBD (UC vs CD), smoking status or when comparing females 50 years or older vs the rest of the group (p>0.05 for all). Moreover, there were no differences in TBS between patients who did or did not engage in resistance exercises (p=0.22) and/or regular aerobic exercises (RAPA ≥6) (p=0.84).
Conclusion
Patients with IBD present with lower TBS Z-scores when compared to HC and there is no correlation with disease activity. The only variable associated with lower TBS was a 25OHD <28 ng/mL. Further studies looking at the implications of these findings are warranted.
FIGURE 1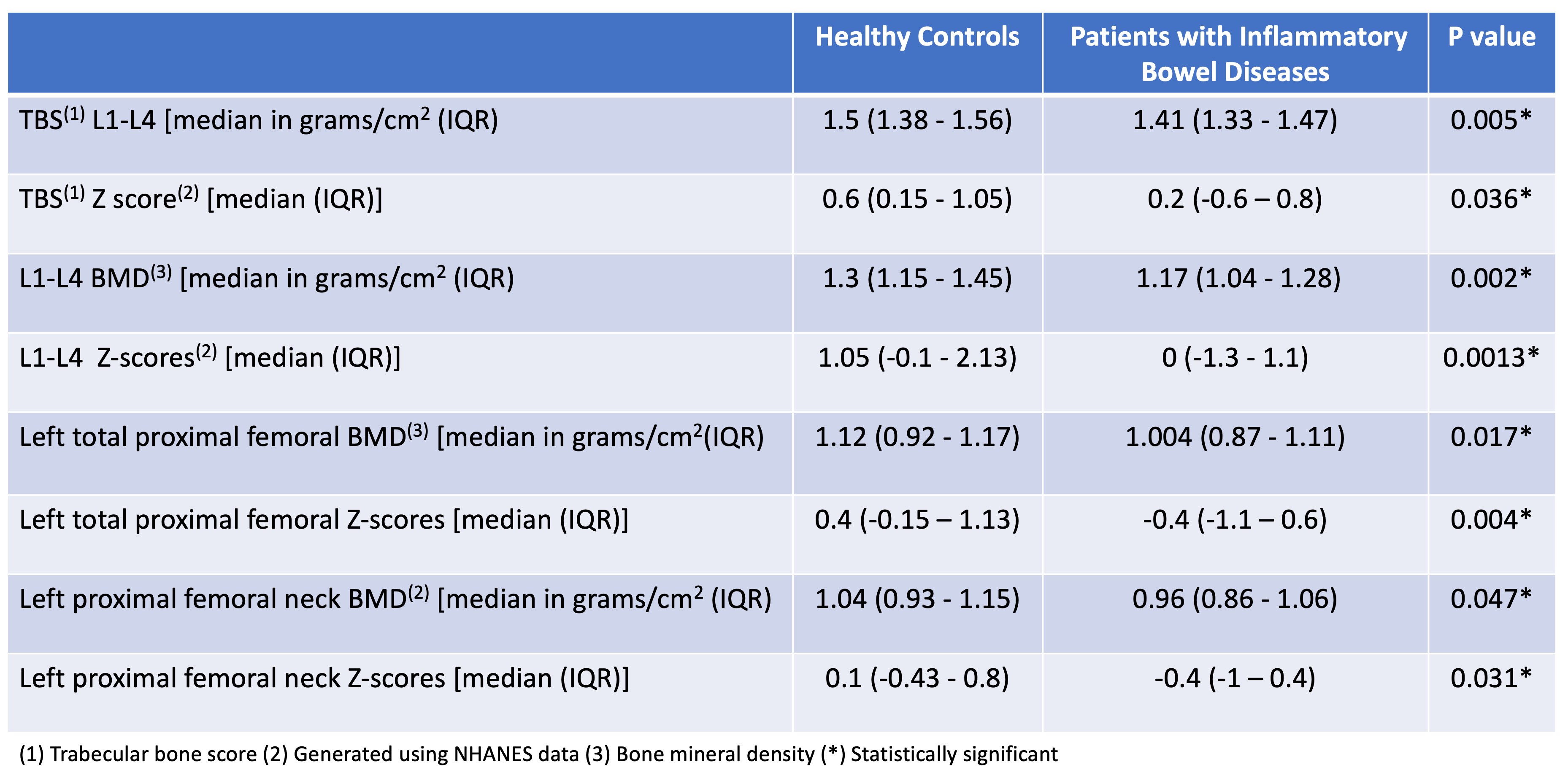
FIGURE 2