P160 Influence of sarcopenia on perioperative management and postoperative outcome in patients with Crohn’s Disease undergoing intestinal surgery: a retrospective study
O'Neill, C.(1,2)*;Haenen, S.(1,3);Coudyzer, W.(4);Bislenghi, G.(5);D'Hoore, A.(5);Verstockt, B.(1);Ferrante, M.(1);Vermeire, S.(1);Sabino, J.(1);
(1)University Hospitals Leuven- KU Leuven, Department of Gastroenterology and Hepatology & Department of Chronic Diseases and Metabolism CHROMETA- Translational Research in GI disorders, Leuven, Belgium;(2)Centro Hospitalar Lisboa Ocidental, Department of Gastroenterology and Hepatology, Lisboa, Portugal;(3)Regional Hospital Heilig Hart, Department of Gastroenterology and Hepatology, Leuven, Belgium;(4)University Hospitals Leuven- KU Leuven, Department of Radiology, Leuven, Belgium;(5)University Hospitals Leuven- KU Leuven, Department of Abdominal Surgery, Leuven, Belgium;
Background
Sarcopenia (loss of skeletal muscle mass and/or strength) is a predictor of postoperative morbidity in various surgical populations. We evaluated the impact of sarcopenia in postoperative outcomes after intestinal surgery in patients with Crohn’s disease (CD) at a tertiary referral centre.
Methods
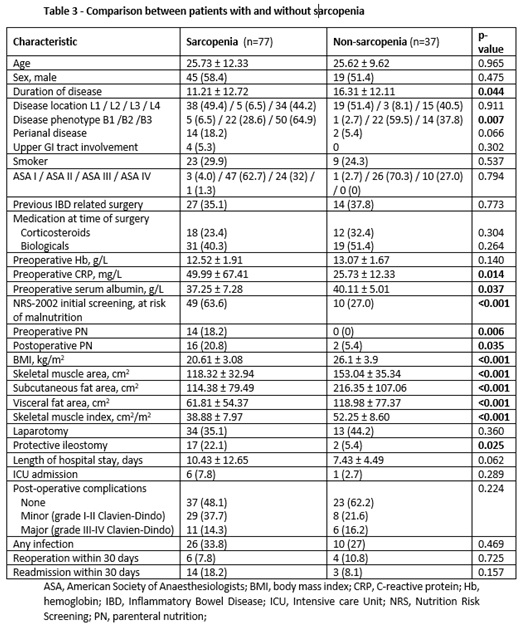
This is a retrospective analysis of all patients with CD undergoing intestinal surgery at our centre, between January 2013 and September 2019 with available abdominal computed tomography images within 90 days before surgery. The images were assessed for sarcopenia according EWGSOP2 criteria (Skeletal Muscle Index <39 cm2/m2 for female and <55 cm2/m2 for male) and visceral and subcutaneous fat areas. All patients were coded for postoperative complications using the Clavien–Dindo classification system.
Results
A total of 114 patients with Crohn’s disease were included (table 1 and 2). The prevalence of sarcopenia was 67.5%. Common intestinal procedures were ileocecal resections (49%), segmental small-bowel resections/stricturoplasty (6.1%), and colon resection (8.8%). Sarcopenic patients have more frequently penetrating phenotype than patients without sarcopenia (p=0.007). Body mass index and serum albumin levels were significantly lower (p<0.001 and p=<0.037, respectively) and C-reactive protein levels were significantly higher (p=0.014) in sarcopenic patients compared to non-sarcopenic patients. Furthermore, both visceral and subcutaneous fat were significantly lower (both p<0.001) in patients with sarcopenia. ICU admission, rates of postoperative complications within 30 days, infections, reoperation and re-hospitalization were not significantly different between sarcopenia and non-sarcopenia groups. However, there was a trend of a longer length of hospital stay (p= 0.062) in patients with sarcopenia. Sarcopenic patients received significantly more preoperative and postoperative parenteral nutrition (p=0.006 and p=0.035, respectively) and protective ileostomy (p=0.025) compared with patients without sarcopenia.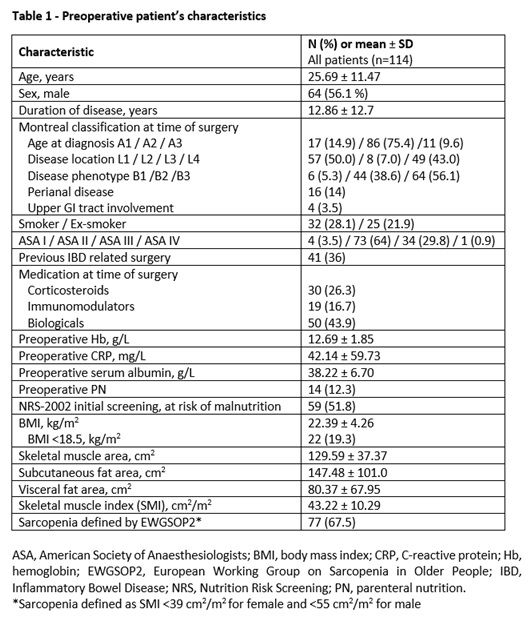

Conclusion
The prevalence of sarcopenia based on EWGSOP2 criteria is high in patients with CD requiring bowel resection. In this cohort, sarcopenia was not linked to higher rate of postoperative complications, although this might be explained by different surgical procedures and nutrition management before and after surgery for CD.


