P175 Low relapse rates after biologic therapy discontinuation in a large real life cohort of IBD patients with initial severe disease: do biologics alter the natural history of disease?
Banerjee, R.(1);Pal, P.(1);Akki, Y.(1);Adigopula, B.(1);Reddy, D.N.(1);
(1)Asian Institute of Gastroenterology, Gastroenterology, Hyderabad, India;
Background
Discontinuation of biologic therapy has been associated with high risk of relapse. However indefinite biologic therapy is often not feasible in low resource settings of the developing countries where tuberculosis (TB) is endemic and cost is prohibitive. There is very limited data on the course of disease after stopping biologics from this region. We analysed the predictors of relapse including the rate and severity post withdrawal of biologics in a large real-world cohort of patients from India.
Methods
Prospectively collected data of consecutive patients treated with biologics from the IBD registry of a large tertiary care centre from India was analyzed. Demographic and disease characteristics, reasons for biologic discontinuation and relapse rate and severity post withdrawal including its management were analyzed. Cox proportional hazard analysis was done to identify predictors of relapse.
Results
403 patients (Median age-35 yrs, range 6-75, 62.5% male, 58% Crohn’s disease:CD, 42% Ulcerative colitis:UC) received biologics for moderate-severe disease (steroid dependent or with complications) with a median follow up of 23 months (IQR-7-48 m, range- 3-228 m). 274 patients (68%) discontinued biologics. 77(28 %) were primary or secondary non-responders. 65 (24%) stopped due to financial constraints. 98 (36%) stopped after clinical and/or endoscopic remission. The other reasons included TB reactivation 8 (2.6%), non-TB infection-5 (2%); infusion reactions: 4 (1.5%); non compliance 14 (5%), aggravated psoriasis 2(1%) and death(1).
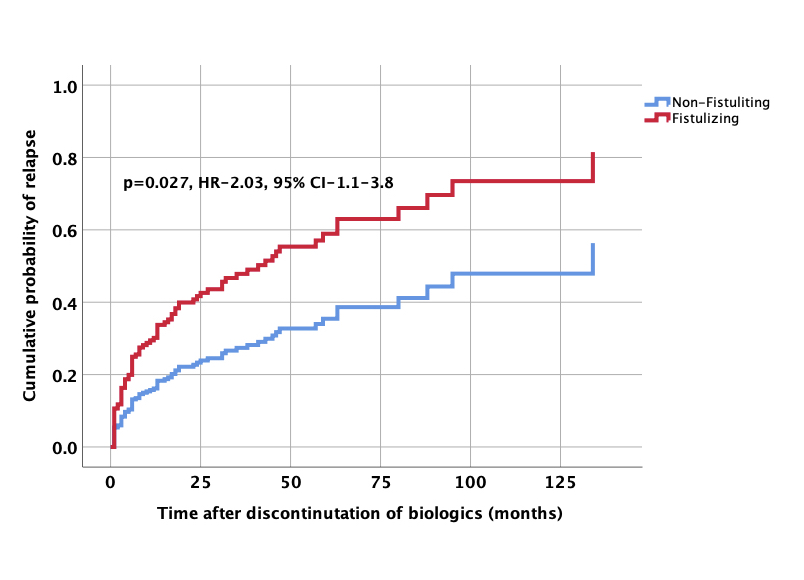
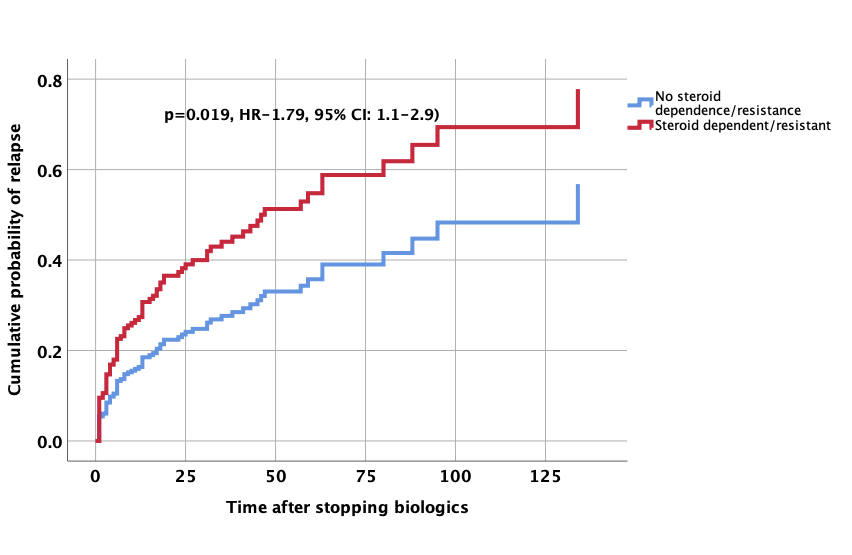
87/274 (32%) relapsed after stopping biologics. 187/274 (68%) were in remission over a median follow up of 24 months (IQR: 10-51 months). 52/87(60%) relapsed in first year and 67/87(77%) in 2 years. Most relapses were mild and responded to steroids 43 (49.4%) or re-treatment with biologics 34 (39%). 10 patients (11%) needed surgery. On Cox proportional hazard analysis, perianal/fistulizing disease (HR-2.03, 95% CI-1.1-3.8, p=0.027) and steroid dependent/resistant disease (HR-1.79, 95% CI-1.1-2.9, p=0.019) were associated with a higher risk of relapse after withdrawal of therapy. Patients who stopped after clinical and endoscopic remission had lower likelihood of relapse after biologics discontinuation(HR-0.48, 95% CI-0.29-0.80, p=0.005).


Conclusion
The relapse rates on discontinuation of biologic therapy was low in patients with clinical and endoscopic remission particularly in non-fistulizing, disease. Most relapses were mild. Majority of the patients with an initial severe disease had a milder course post withdrawal of biologic therapy suggesting that biologics could alter the natural course of the disease. Further multi-centre and long term studies are warranted.


