P179 Distinct ultrasound characteristics of the appendix in patients with ulcerative colitis: a prospective, cross-sectional cohort study
Reijntjes, M.(1);de Voogd, F.(2);Bemelman, W.(1);d'Haens, G.(2);Buskens, C.(1);Gecse, K.(2);
(1)Amsterdam UMC- location AMC, Surgery, Amsterdam, The Netherlands;(2)Amsterdam UMC- location AMC, Gastroenterology, Amsterdam, The Netherlands;
Background
Increasing evidence suggests a role for the vermiform appendix in onset and relapse of ulcerative colitis (UC). Consequently, appendectomy is increasingly being seen as a potential alternative treatment. As a recent study suggests that patients with histological appendiceal inflammation are most likely to respond, pre-operative identification of ulcerative appendicitis could be beneficial1. Intestinal ultrasound (IUS) is increasingly utilized in the diagnosis and follow-up of patients with UC. The objective of this study was to characterize the appendix by IUS in UC patients with active and quiescent disease and healthy controls.
Methods
In this cross-sectional prospective observational cohort study, we performed appendiceal IUS on UC patients with active (A) disease (FCP>250 and SCCAI>5) and quiescent (Q) disease (FCP<150 and SCCAI<5), followed by age-, body mass index- and gender- matched healthy (H) controls. During IUS, the appendix was identified as a bowel structure with cecal origin and a blind-ending tip. IUS still images and cineloops were centrally and blindly read by an IUS expert (>1000 examinations). Primary outcomes were signs of appendicitis on IUS, defined as a <6 mm transverse appendiceal diameter3 (average of a cross-sectional and longitudinal measurement), hyperaemia (using the modified Limberg score2), presence of peri-appendiceal fat and fluid, and compressibility.
Results
Out of 95 (A n=35, Q n=30, H n=30) included patients, the majority (n=58, 61.1%) had a visible appendix on IUS, which was similar among cohorts (p=0.56). The appendiceal diameter measured >6.0mm in a significantly higher proportion of active UC patients (A: 45.5%, Q: 5.6%, H: 0.0%, p=0.01). An increased diameter occurred irrespective of disease extent (42.9% of E1/E2 endoscopic active patients). Although the appendiceal diameter was higher for UC patients (Q-H p= 0.02, A-H p< 0.01), no significant difference between A and Q patients was found (p=0.15, Fig. 1). A higher proportion of UC patients had incompressibility when compared to healthy controls (Fig. 2a, p= 0.02). Hypervascularity was present in 54.5% of active UC (Fig. 2b, p= 0.02).
Fig 1. Box plot of appendiceal diameter (mm) among cohorts
Fig 2 (a, b). Bar charts of incompressibility (a) and hypervascularity (b) among cohorts
a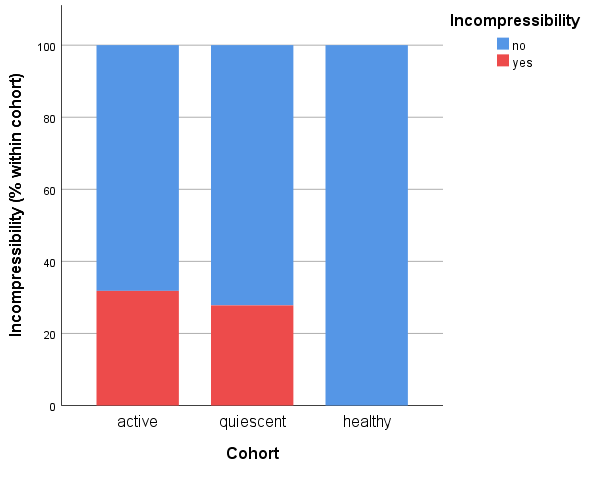
b
Conclusion
Appendiceal IUS was feasible in UC patients. Characteristics of appendiceal inflammation of IUS were reported for UC patients, as both the transverse appendiceal diameter and incompressibility rates were significantly higher in UC patients when compared to healthy controls. Correlating appendiceal IUS findings to histological inflammation could contribute to identifying UC patients most likely to benefit from appendectomy.