P193 Correlation of the IBD Disk scores with diagnosis of IBD, Faecal calprotectin and Endoscopic scores in patients presenting to a rapid access IBD inception clinic.
Shariff , S.(1);Sharma , N.(1);Quraishi , M.N.(1);Cooney , R.(1);Iqbal , T.(1);Rimmer , P.(1);
(1)Department of Gastroenterology- University Hospitals Birmingham NHS Foundation Trust- Birmingham- UK, Gastroenterology, Birmingham, United Kingdom;
Background
The IBD-Disk was adapted from the Inflammatory Bowel Disease –Disability Index as a tool to capture a patient's functional status for Health Care Professionals to review. Patients complete this disk for ten symptoms with scores ranging from 0 to 10. Patients with higher scores have a significant burden of disease. We explore correlation of IBD disk score with faecal calprotectin, endoscopic scores, and a diagnosis of IBD in patients referred to our inception clinic service.
Methods
Patients with symptoms compatible with Inflammatory Bowel Disease (IBD) and a raised faecal calprotectin are fast tracked to our rapid access inception clinic service for further assessment. We prospectively collected data on demographics, faecal calprotectin levels and IBD disk scores. We assessed correlation between the total score and individual components of the IBD disk score with demographics, faecal calprotectin (F.Cal) at presentation and subsequent diagnosis of IBD and endoscopic scores. Descriptive and multivariate regression analysis was performed.
Results
68 patients (47% female; median age 35.5 years [IQR 16.8]) attending the inception clinic were included in this analysis. Of these patients 17/68 (25%) were diagnosed with Crohn’s disease (CD), 18/68 (26%) with ulcerative colitis (UC) and 5/68 (7%) with indeterminate colitis. 33 (33.8%) had unclear diagnoses and are currently undergoing further investigation. IBD was excluded in 5/68 (7%) patients. Younger patients (age 15 – 30 years) and patients above 60 years of age had a relatively higher F.Cal at presentation (Figure 1).
The total IBD disk score was significantly higher in younger patients (p=0.03). No correlation was seen between the eventual diagnosis of IBD and total score at presentation or individual components of the IBD disk score. Multivariate regression analysis, however, demonstrated significant correlation between regulated defecation and interpersonal interactions with F.Cal at baseline in patients with IBD (p<0.05). No correlation was seen with other variables of the IBD disk and faecal calprotectin levels.
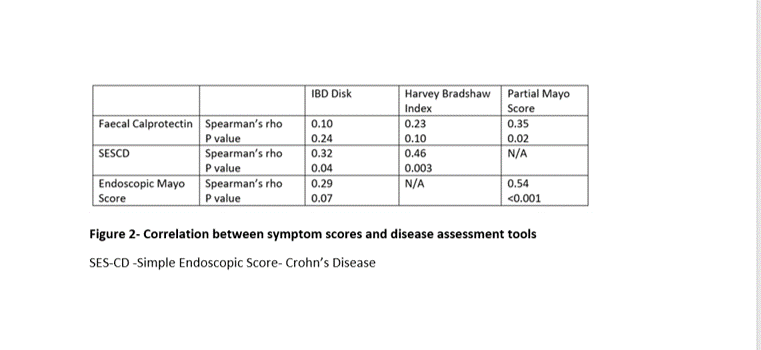
IBD Disk score as well as Harvey Bradshaw index correlated well with Simple Endoscopic Score in Crohn’s disease (SES-CD) (Figure 2). No significant correlation was seen between IBD Disk score and baseline F.Cal or Endoscopic Mayo Score . The simple Mayo score showed a better correlation between F.Cal and Endoscopic Mayo score than IBD Disk. 
Conclusion
Correlation of F.Cal with certain elements of the IBD Disk tool highlights its utility in capturing both inflammatory and non-inflammatory related disability in patients with IBD. IBD Disk Scores correlate with CD endoscopic severity scores (ie SES-CD) but not UC scores ( ie Endoscopic Mayo Score).


