P197 Anogenital Crohn’s disease and granulomatosis: A systematic review of epidemiology, clinical manifestations, and treatment
Honap, S.(1);Meade, S.(1);Spencer, A.(2);Pavlidis, P.(1);Luber, R.(1);Calonje, E.(3);Rashid, E.(4);Bunker, C.(5);Lewis, F.(3);Irving, P.(1);
(1)Guy's and St Thomas' NHS Foundation Trust, IBD Centre- Department of Gastroenterology, London, United Kingdom;(2)Hammersmith Hospital- Imperial College Healthcare NHS Trust, Department of Dermatology, London, United Kingdom;(3)Guy’s and St Thomas’ NHS Foundation Trust, Department of Dermatopathology- St John's Institute of Dermatology, London, United Kingdom;(4)Guy’s and St Thomas’ NHS Foundation Trust, St John's Institute of Dermatology, London, United Kingdom;(5)University College London Hospitals NHS Foundation Trust, Dermatology Department, London, United Kingdom;
Background
Metastatic Crohn’s disease (CD) is an extra-intestinal manifestation (EIM) characterised by ulceration, swelling or inflammatory lesions that are non-contiguous with the gut; genital involvement is rare. We conducted a systematic review of ACD and granulomatosis to provide a synthesis of epidemiology, clinical features, and treatment outcomes in adults and children.
Methods
A systematic literature search was conducted via MEDLINE, EMBASE and the Cochrane database from inception to 1st December 2020 to identify studies of ACD presentation and/or treatment outcomes. Investigators extracted, analysed, and reported study data in accordance with PRISMA. Clinical response was defined as a reduction in symptoms, genital swelling or partial healing of ulcers and fissures. Remission was defined as complete resolution of symptoms and examination findings.
Results
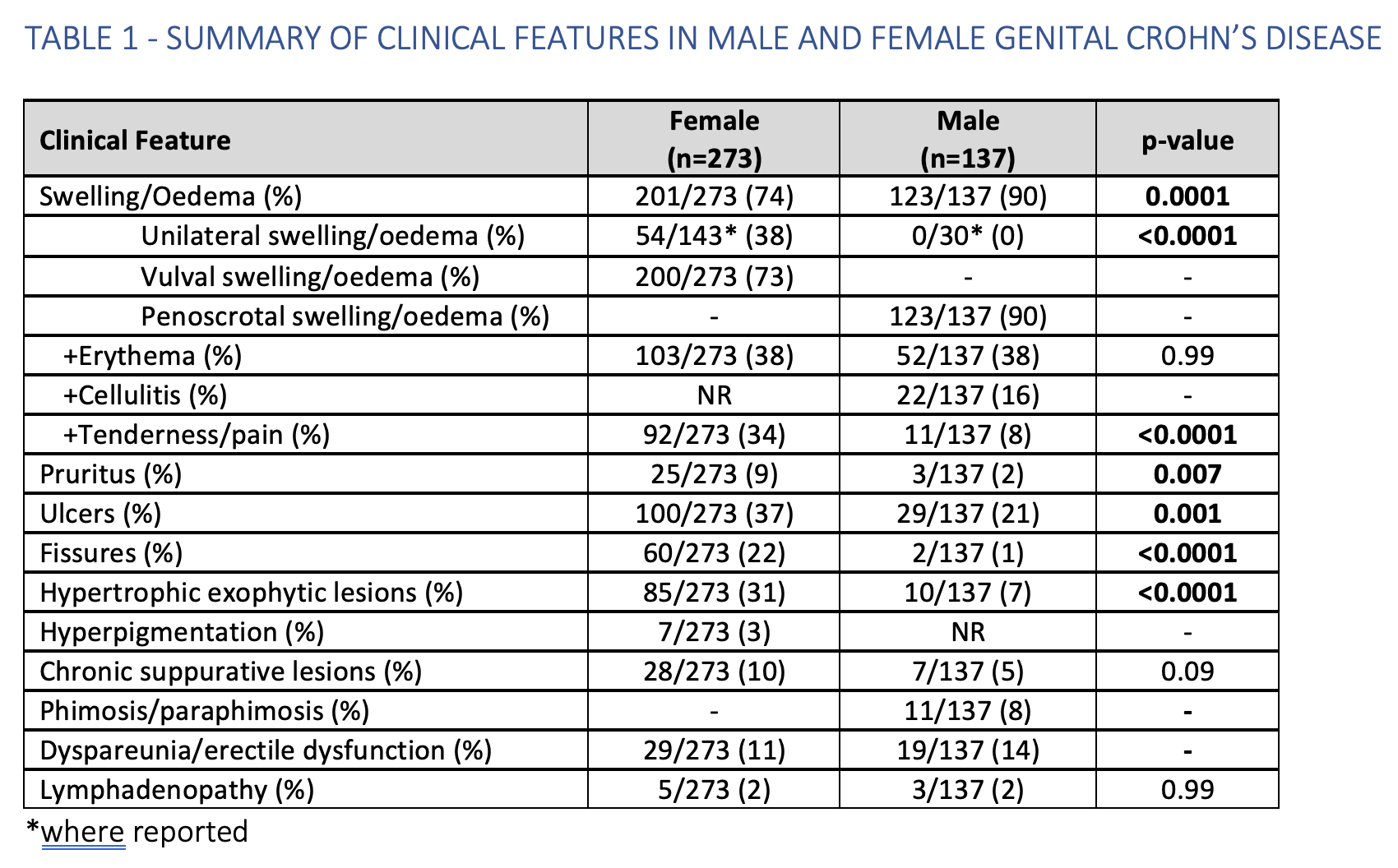
Of 9,381 screened studies, 185 articles, (comprising 410 cases; 273 female (F), 137 male (M)), were included (figure 1). The median age at diagnosis was 29 (F) and 16 (M) and up to 50% did not have a prior CD diagnosis. Luminal CD was subsequently diagnosed in 80% of cases including 45-80% patients without gastrointestinal symptoms (time to CD diagnosis from ACD presentation [range] –43 to 11 years). The predominant clinical features across both sexes were, oedema (79%), ulcers/fissures (47%), and hypertrophic, exophytic lesions (nodules and plaques) (23%) (table 1). Adults and children present similarly. Most patients, 81% (331/410), underwent genital biopsy (106 (M), 225 (F)). Granulomas were noted in 71% (234/331) cases and an inflammatory cell infiltrate was documented in 191/331 (58%). Systemic antibiotics, corticosteroids, thiopurines and anti-TNF therapy were the most frequently prescribed agents with the highest response and remission rates (table 2). At final follow-up, where reported, non-response, response, and remission rates were 37/304 (12%), 267/304 (88%) and 114/304 (38%), respectively. Oedema was associated with a poor response to topical corticosteroids vs. those with ulcers or fissures without oedema (p=0.03). Greater response rates to anti-TNF therapy were seen in patients prescribed concomitant immunomodulation (24/25, 96% vs 67/90, 74%, p=0.02).
Conclusion
To our knowledge this is the first systematic review of ACD in adult and paediatric males and females. ACD and granulomatosis are rare EIMs of CD that are under-recognised, leading to treatment delay, and significant morbidity. There is a wide heterogeneity in presentation and some of the treatments used in luminal and perianal CD appear to be effective. Further studies with longer follow up are required to define optimal treatment strategies.