P204 Endotrophin (PRO-C6) is associated with MRE confirmed intestinal strictures and Protein FingerPrint biomarkers of collagen degradation is associated with ulcerations in paediatric Crohn’s disease patients – results from the ImageKids study
Mortensen, J.(1);Focht, G.(2);Pehrsson, M.(1);Griffiths, A.M.(3);Alexdóttir, M.S.(1);Church, P.C.(3);Baldassano, R.N.(4);Bay-Jensen, A.C.(1);Silverstein, J.(5);Karsdal, M.A.(1);Turner, D.(2);
(1)Nordic Bioscience A/S, Biomarkers & Research, Herlev, Denmark;(2)Shaare Zedek Medical Center, Pediatric Gastroenterology and Nutrition Unit, Jerusalem, Israel;(3)Hospital for Sick Children, Division of Gastroenterology, Toronto, Canada;(4)The Children's Hospital of Philadelphia, Division of Gastroenterology- Hepatology- and Nutrition, Philadelphia, United States;(5)Harvard Medical School, Division of Gastroenterology- Hepatology and Nutrition, Boston, United States;
Background
Most patients with inflammatory bowel disease (IBD) eventually develop intestinal fibrosis due to increased extracellular matrix (ECM) remodelling. There is a huge medical need for non-invasive serological biomarkers for intestinal fibrosis and inflammation, as magnetic resonance enterography (MRE) and endoscopy are less desirable for repeated monitoring. Therefore, we aimed to investigate Protein FingerPrint assays (PFA) of collagen remodelling and citrullinated vimentin as surrogate markers of intestinal stenosis and tissue inflammation in paediatric Crohn’s disease (pCD) patients.
Methods
This is a proteomics planned sub-study of the multi-center prospective ImageKids study that enrolled children with CD undergoing MRE and colonoscopy concurrently (ImageKids study: NCT01881490). We included those in Tanner stage 5 with available serum sample for these initial analyses, as age and stage of physical development affects ECM remodelling. Serum from healthy age and gender matched controls were obtained from Central BioHub. PFA biomarkers of collagen degradation (C1M, C3M, C4M, C6M), collagen formation (PRO-C1, PRO-C3, PRO-C4, PRO-C5, PRO-C6) and citrullinated vimentin (VICM) were measured. Intestinal stenosis was determined by MRE and mucosal inflammation by the SES-CD. Student’s t-test, Pearson r correlation and one-way-ANOVA with Tukey correction was applied for statistical analysis.
Results
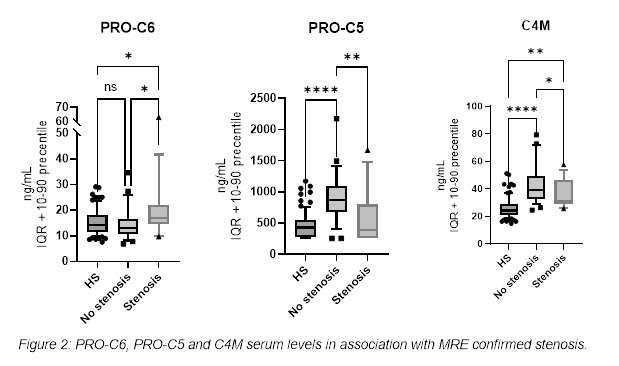
50 pCD adolescents were included (mean age ± 14.53 years, 30 (60%) females, 11 (22%) in clinical remission and 18 (36%) with moderate-severe disease), along with 83 serum samples from healthy controls. SES-CD correlated with C1M (r=0.58, p=0.0001), C3M (r=0.46, p=0.0033), C6M (r=0.48, p=0.0021), PRO-C4 (r=0.58, p=0.0001), VICM (r=0.48, p=0.0018), PRO-C1 (r=-0.39, p=0.015) and PRO-C3 (r=-0.33, p=0.043). C1M (p<0.0001), C3M (p<0.05), and C6M p<0.001) were elevated in patients with severe ulcers compared to patients without ulcers, and vice versa for VICM (figure 1). PRO-C6 (p<0.05) was significantly elevated between patients with vs. without intestinal stenosis, and PRO-C5 (p<0.01), C4M (p<0.05), and PRO-C4 (p<0.05) were significantly lower (figure 2).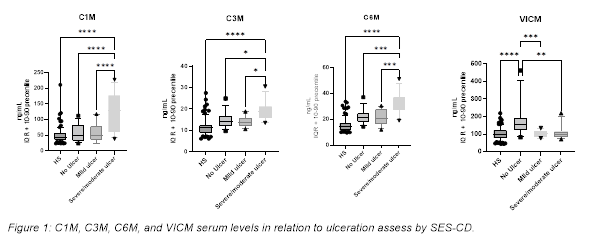
Conclusion
PFA biomarkers of collagen degradation and formation are associated with inflammation and/or intestinal fibrosis pCD. Furthermore, the biomarkers C1M, C3M, C4M, C6M, reflecting mucosal damage and tissue inflammation, were elevated in pCD patients with severe ulcers. PRO-C6, PRO-C5 and C4M were the best PFA biomarkers to reflect MRE-confirmed stenosis. PFA biomarker of collagen remodelling could potentially be applied as surrogate biomarkers for monitoring of mucosal damage/tissue inflammation and fibrostenotic stricture development.


