P208 Correlation between physician and patient disease assessments in ulcerative colitis: 2-year UK data from the ICONIC study
N. Bhala1, A. Hart2, D. Watts3, S. Lewis4, S. Ghosh5, S. van Haaren6, C. Hansell6, T. Ahmad7
1Department of Gastroenterology, Queen Elizabeth Hospital Birmingham, Birmingham, UK, 2St Mark’s Hospital, IBD Unit, Harrow, UK, 3Department of Gastroenterology, NHS Forth Valley, Stirling, UK, 4Department of Gastroenterology, Plymouth Hospitals NHS Trust, Plymouth, UK, 5Department of Gastroenterology, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK, 6AbbVie Ltd., Medical, Maidenhead, UK, 7Department of Gastroenterology, Royal Devon and Exeter Hospital, Exeter, UK
Background
ICONIC is the largest prospective multi-country (
Methods
Adults with early UC (diagnosed ≤36 months) were enrolled irrespective of disease severity or treatment. Patient self-assessments include disease severity, Pictorial Representation of Illness and Self-Measure (PRISM, a tool assessing perception of disease-associated suffering; lower scores indicate greater disease burden), Patient Health Questionnaire-9 (PHQ-9), Short inflammatory bowel disease Questionnaire (SIBDQ) and patient-modified Simple Clinical Colitis Activity Index (P-SCCAI). Physician assessments include clinical parameters, PRISM, SCCAI. Correlation between PRISM and SIBDQ, PHQ-9 and SCCAI were evaluated by Spearman correlation. BL characteristics are based on observed data.
Results
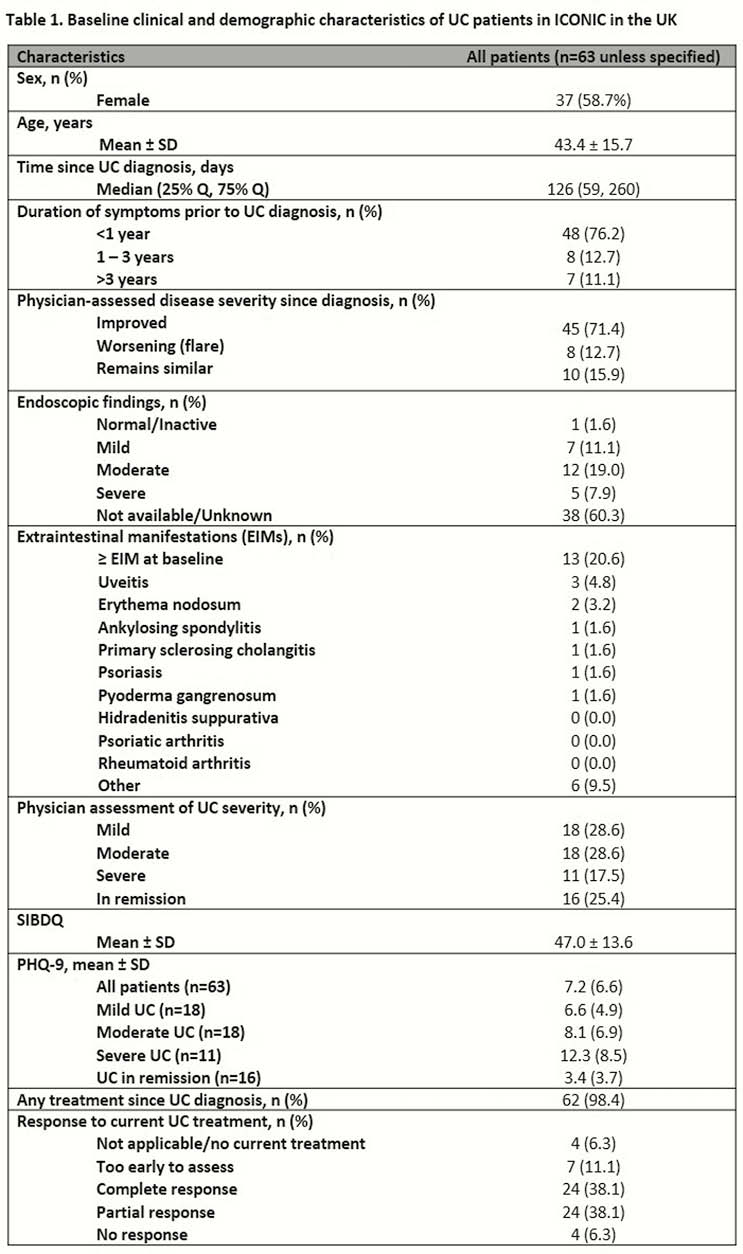
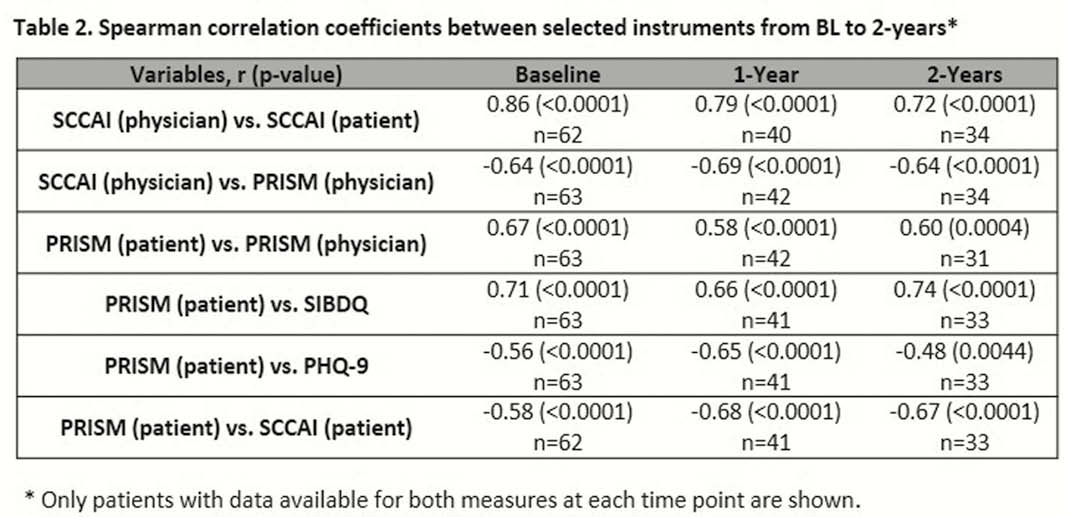
BL characteristics of 63 UK patients in ICONIC are shown in Table 1. From BL to 2-years, patient/physician PRISM was moderately/strongly correlated with SIBDQ, PHQ-9, P-SCCAI or SCCAI (Table 2). For 62 patients with self and physician assessments, the level of agreement on disease severity at BL (concordant pairs) was: mild 66.7%, moderate 27.8%, severe 45.5%, in remission 50.0%. The mean ± SD P-SCCAI and physician SCCAI values at 2 years were 2.6 ± 2.6 and 1.5 ± 1.5, respectively; the measures were strongly correlated (Table 2). For patient/physician PRISM assessments at 2 years, scores were 5.2 ± 2.6 and 5.2 ± 2.1, respectively, and were moderately/strongly correlated (Table 2).
Conclusion
Results from this subanalysis of ICONIC demonstrate persistently high UC disease burden over 2-years, despite treatment. EIMs were common and therefore awareness of potential EIM impact is essential. PRISM, used for the first time in UC, was moderately correlated with disease-specific measures (SIBDQ/SCCAI) and a general depression assessment (PHQ-9). Alignment between patients and physicians on disease activity/severity varied according to the instrument used but was greatest for SCCAI.


