P225 The accuracy of different intestinal ultrasound parameters in detecting endoscopic activity in patients with inflammatory bowel disease
KatsarosMD, M.(1)*;Palmela, C.(2);Kalogirou, M.(1);Frias Gomes, C.(2);Katsoula, A.(1);Torres, J.(2);Giouleme, O.(1);
(1)Hippokration Hospital, Gastroenterology Division- Second Propaedeutic Department of Internal Medicine- Medical School- Aristotle University of Thessaloniki, Thessaloniki, Greece;(2)Hospital Beatriz Ângelo, Department of Gastroenterology, Loures, Portugal;
Background
Intestinal ultrasound (IUS) is considered an accurate tool for assessment of disease activity in inflammatory bowel disease (IBD) patients. We investigated the accuracy of IUS to detect active disease as compared to ileocolonoscopy.
Methods
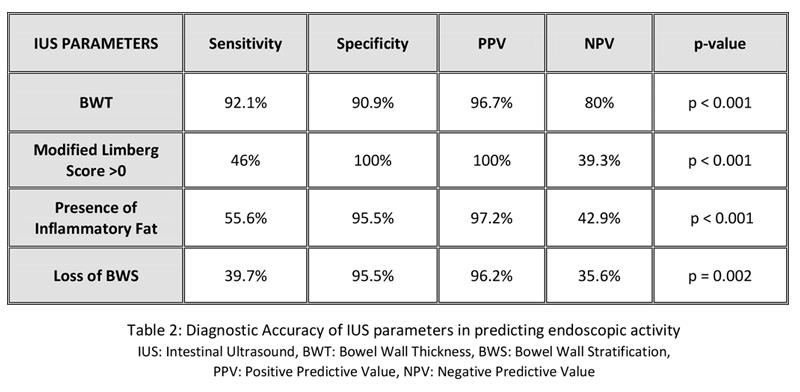
We performed a two-center international cross-sectional study that included formally diagnosed IBD patients who underwent IUS and ileocolonoscopy, within a 4 weeks interval. Active disease on IUS was defined as bowel wall thickness (BWT) >3 mm in the most affected bowel segment. Additional IUS parameters evaluated included increase in Doppler color flow in the bowel wall (modified Limberg score > 0), presence of inflammatory fat (FW) and loss of bowel wall stratification (BWS). Active disease at endoscopy was defined as Simple Endoscopic Score for Crohn’s Disease (SES-CD) >2 and Mayo endoscopic score >0. The accuracy of IUS compared to ileocolonoscopy was estimated using sensitivity, specificity, and Cohen’s kappa coefficient analyses.
Results
We included 85 patients (table 1) performing IUS for disease monitoring (69.4%) and symptoms suggestive of IBD flare (30.6%). Disease was active in IUS in 38/42 (90.5%) of clinically active [Harvey Bradshaw index (HBI) ≥5, Simple Clinical Colitis activity index (SCCAI) >2] and 22/43 (51.2%) of clinically inactive patients (kappa coefficient 0.391, p<0.001). C-reactive protein (CRP) level was 6.95 mg/dl [IQR 2.19-17.75] vs 1.8 mg/dl [IQR 0.85-3.75] in active vs inactive disease on IUS respectively (p<0.001). All patients underwent both endoscopy and IUS, with 63/85 (74.1%) exhibited endoscopic activity. IUS demonstrated 92.1% sensitivity, 90.9% specificity, 96.7% PPV, 80% NPV and kappa coefficient 0.79 in detecting endoscopically active disease (p<0.001). IUS detected 58/63 (92.1%) of endoscopically active cases, and identified the most affected bowel segment in 50/63 (79%) of them. Inability of IUS to identify the most affected bowel segment at endoscopy included rectal involvement (53.8%), complex surgical history (15.38%), stenosis of ileocecal valve (7.69%) and limitations due to obesity (23.07%). Mean BWT of the most affected segment was 4.49 (±1.16) vs 2.33 mm (± 0.63) in endoscopically active vs inactive patients respectively (p<0.001). We furthermore evaluated the accuracy of additional IUS parameters (increased color Doppler flow, FW and loss of BWS) in predicting endoscopic activity (table 2).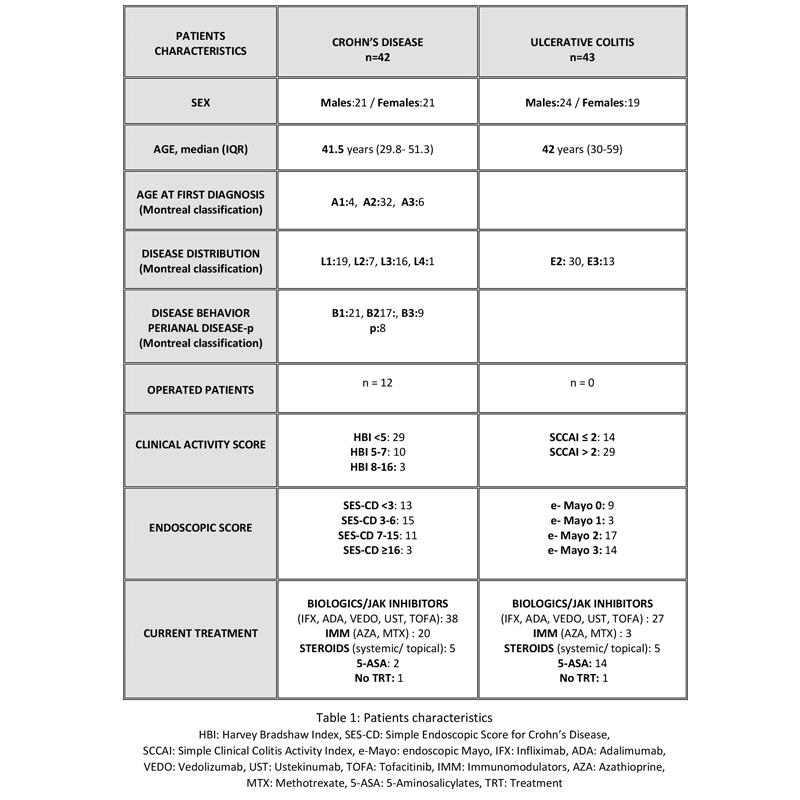
Conclusion
IUS represents a non-invasive tool that can accurately identify disease activity both in Crohn’s disease and ulcerative colitis, when compared to ileocolonoscopy. The most sensitive parameter to detect endoscopic activity was an increased BWT.


