P227 Defining faecal calprotectin thresholds to predict endoscopic and histological healing in ulcerative colitis (UC) by using advanced optical enhancement techniques
R. Cannatelli1,2, D. Zardo3, O. Nardone1, A. Bazarova4, U. Shivaji1,5, S.C.L. Smith1,5, S. Ghosh1,5,6, M. Iacucci1,5,6
1Institute of Translational Medicine, University of Birmingham, Birmingham, UK, 2Department of Gastroenterology, Milan, Italy, 3Department of Histopathology, Birmingham, UK, 4Institute for Biological Physics, Cologne, Germany, 5University of Birmingham, NIHR Biomedical Research Centre, Birmingham, UK, 6University of Calgary, IBD Unit, Calgary, Canada
Background
Faecal calprotectin (FC) is the most common surrogate marker of mucosal healing (MH) in UC. A number of endoscopic and histologic scoring systems in UC have been developed for defining MH. We report the optimum FC thresholds for defining MH using all the assessment methods.
Methods
In a prospective study we collected all clinical, endoscopic and histologic data and FC from 76 UC patients (mean age 44.2y, 50.0% male) who attended endoscopy unit for colitis assessment or surveillance. Endoscopic scores were determined by the same endoscopist (MI) and included Mayo Endoscopic Score (MES), Ulcerative Colitis Endoscopic Index of Severity (UCEIS) and PICaSSO (Paddington International virtual ChromoendoScopy ScOre). Histological activity was scored by the Robarts Histology Index (RHI) and Nancy Index by the same pathologist (DZ). Faecal calprotectin was assayed using Buhlmann faecal turbo test, particle enhanced turbidimetric immunoassay. ROC curves were performed to evaluate sensitivity, specificity and accuracy of the optimum cut-off of FC to predict endoscopic and histological healing.
Results
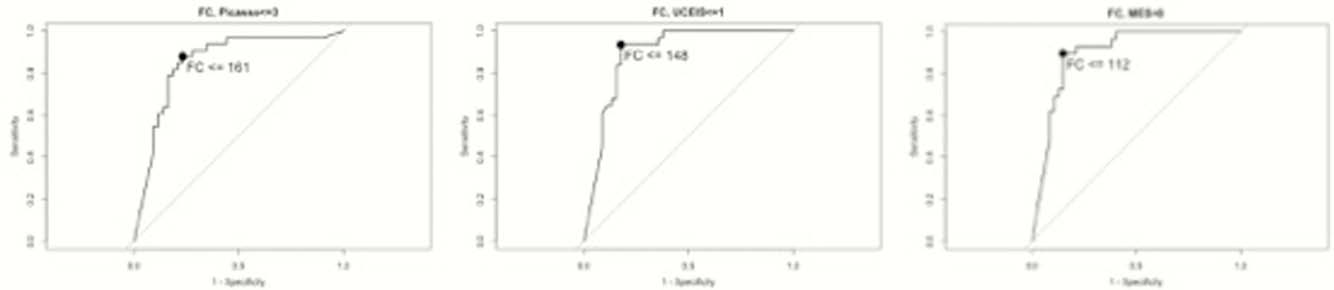
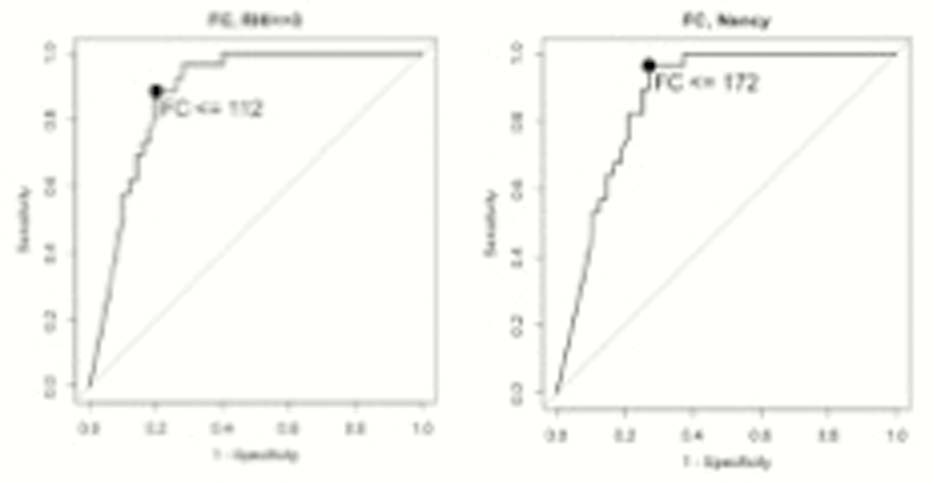
The best cut-off for FC to predict endoscopic healing calculated as Picasso≤3 was 161 μg/g with Area Under ROC curve (AUROC) of 85.3% (95% CI 76.2, 94.4). Sensitivity, specificity and accuracy were 87.9% (95% CI 57.6, 100), 76.7% (95% CI 53.5, 90.7) and 81.6% (95% CI 68.4, 89.5), respectively. While, the best threshold of FC to predict UCEIS≤1 was 148 μg/g with AUROC of 89.2 (95% CI 81.9, 96.5). Sensitivity was 93.5% (95% CI 50.5, 100), specificity 82.2% (95% CI 53.3, 91.1) and accuracy 86.8% (95% CI 69.7, 92.1). The best threshold for FC to predict MES equal to 0, was 112 μg/g, with AUROC of 89.6 μg/g, (95% CI 82.5, 96.7). Sensitivity, specificity and accuracy were 89.7%ww (95% CI 39.2, 100), 85.1% (95% CI 55.3, 93.6) and 86.9% (95% CI 68.4, 92.1), respectively. The best value of FC to predict histological healing with RHI≤3 was 112μg/g with AUROC of 88.0% (95% CI 80.6, 95.4). Sensitivity, specificity and accuracy were 88.5% (95% CI 53.8, 100), 80.0% (95% CI 62.0, 90.0) and 82.9% (95% CI 72.5, 89.5), respectively.
When used Nancy≤1 FC cut-off to predict healing was 172 μg/g with AUROC of 87.1% (95% CI 78.6, 95.6). Sensitivity was 96.4% (95% CI 60.7, 100), specificity 72.9% (54.2, 85.4) and accuracy 81.6% (69.7, 89.5).
Conclusion
Advanced enhancement technologies can accurately define the level of FC to predict endoscopic and histological healing in UC. The optimum FC threshold for MH by PICaSSO and by Nancy was similar (161 and 172 μg/g respectively), while the FC threshold for mucosal healing by MES and by RHI was 112 μg/g. The FC threshold for determining MH in clinical practice should be lower than at least 200 μg/g.


