P230 Adalimumab in Crohn’s disease is protective against periodontitis based on a validated oral health questionnaire
Saravanapavan, H.(1,2)*;Rath, S.(1,2);Inniss, S.(1,2);Ong, M.(1);Sabalić, M.(3);D'Aiuto, F.(3);Rahman, F.(1,2);Smith, A.M.(1);
(1)University College London, Microbial Diseases- Eastman Dental Institute, London, United Kingdom;(2)University College London Hospital, Department Gastroenterology, London, United Kingdom;(3)University College London, Periodontology Unit- UCL Eastman Dental Institute and Hospital, London, United Kingdom;
Background
Crohn’s disease (CD) is associated with a 3-4 fold increased risk of periodontitis compared to the general population1 though periodonitis is poorly recognised and diagnosed. Evidence from mouse models highlight an important link between oral and gut health. Periodontitis has been shown to lead to ectopic colonization of oral pathogens and oral Th17-T cells that activate lamina propria macrophages and exacerbate gut inflammation2. Very little is known about the patient demographics of those at risk of periodontitis. This study aimed to assess the risk factors for periodontitis in CD patients.
Methods
We conducted a cross-sectional study recruiting CD patients at UCLH through myCare, an online platform for patients linked to their clinical records. Patient data were obtained using EpicCare, a web-based electronic patient record database. Patient risk of periodontitis was determined using a previously validated oral health questionnaire3. Statistical tests were conducted using IBM SPSS Statistics 27.
Results
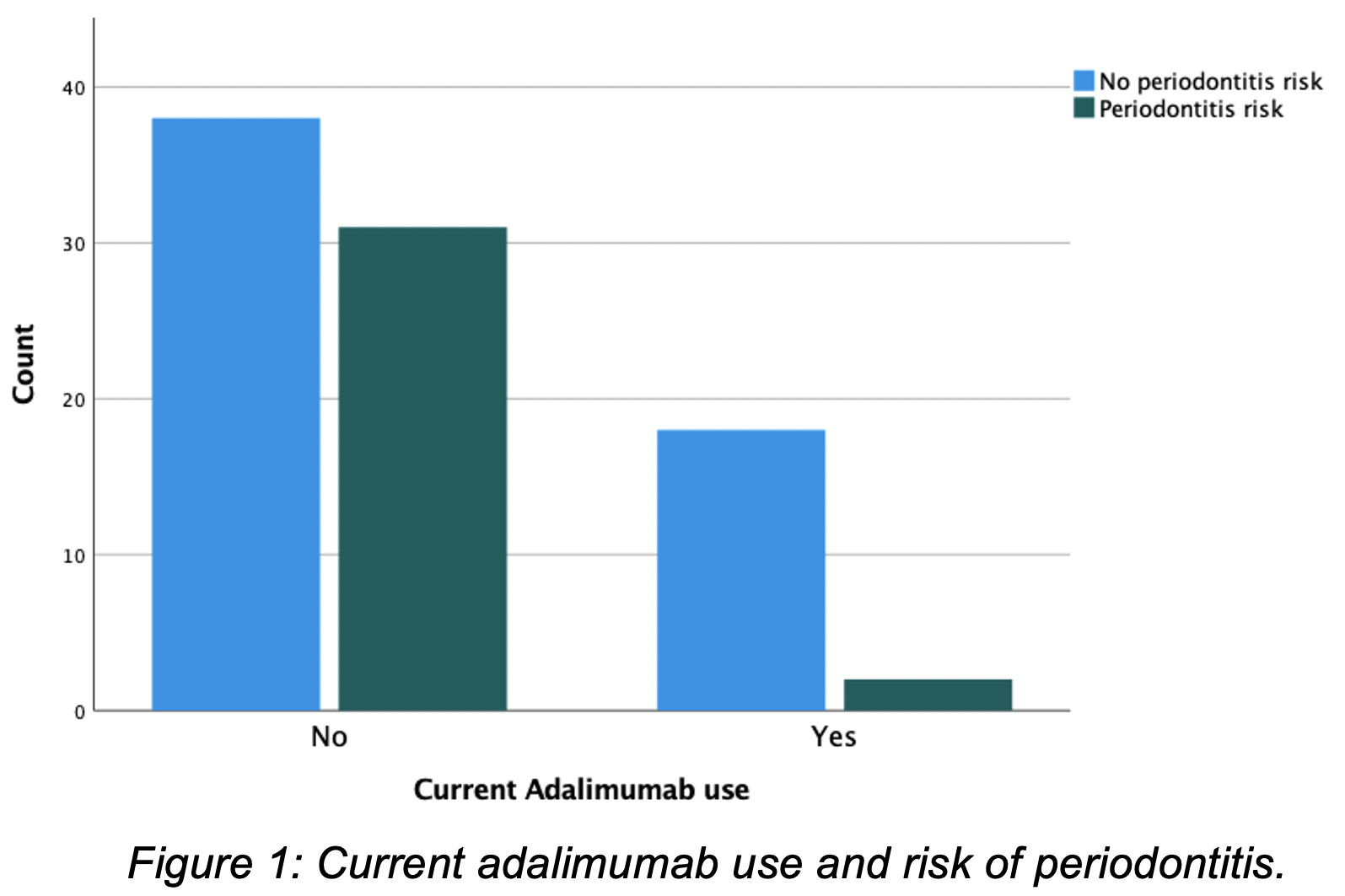
This single centre study included 89 CD patients; 54% female and median age of 40 (IQR 19-82). Patients predominantly identified as White British (56%). The majority had ileocolonic CD (51%) with non-stricturing/non-penetrating behaviour (70%) and were on biologic therapy (52%) (Tab 1). The oral health questionnaire identified 37% of CD patients at risk of periodontitis. There was no statistically significant association between periodontitis risk and age, gender, age at CD diagnosis, disease duration, CD phenotype, family history, body mass index (BMI) or smoking status. Current steroid, immunomodulator use and number of prior biologics also showed no association. Current use of adalimumab and ustekinumab were both independently correlated with risk of periodontitis (χ2 p=0.004 & χ2 p=0.044, respectively). 90% of patients receiving adalimumab were not at risk of periodontitis (Fig 1). In contrast, 60% of patients on ustekinumab were at risk of periodontitis. Logistic regression analysis showed that patients receiving adalimumab were 86% less likely to be at risk of periodontitis compared to patients not receiving adalimumab (OR 0.14 (CI 0.029 - 0.633, p=0.011)). 75% of the adalimumab group was anti-TNF naïve, but no association was seen between prior biologic use and periodontitis risk (p=0.91).
Conclusion
The questionnaire has identified a third of patients who are at risk of periodontitis in the CD cohort. Adalimumab shows benefit in mitigating this risk and may be a drug of choice in patients with oral disease. The questionnaire is a helpful tool to identify and refer at-risk patients.


