P231 Emergency Colectomy for IBD Is Not Associated with Increased Risk of Postoperative Infection, Reoperation or Readmission
Connelly, T.(1);Clancy, C.(1);Cheong, J.Y.(1);Jia, X.(1);Kessler, H.(1);Valente, M.(1);HolubarMD- MS, S.(1);
(1)Cleveland Clinic, Department of Colon & Rectal Surgery, Cleveland, United States;
Background
The current literature suggests that IBD patients have worse outcomes after emergency surgery when compared to elective surgery. We hypothesized that this association will be lost after matching cohorts of emergency and elective patients. We aimed to confirm the current emergency IBD surgery literature in a large cohort of unmatched IBD patients. We then aimed to determine if postoperative outcomes are worse in matched patients undergoing elective vs emergency colectomy.
Methods
We utilized the NSQIP PUF IBD Cohort 2005-2019 to assess 30-day outcomes in adult IBD patients undergoing emergency vs elective colectomy. Our primary outcome was any complication. Our secondary endpoints were readmission, reoperation, and mortality. Univariable and multivariable logistic regression models were used to examine the association between emergency surgery and complications in the unmatched cohort. Propensity-score matching was performed to match emergency patients to non-emergency patients on a 1:1 basis. A logistic regression model was used to assign a propensity score to each patient using emergency surgery as the outcome. All preoperative and perioperative characteristics were included in the model except those with > 20% missing data. The probability of emergency surgery based on these factors was used as the propensity score. A greedy matching algorithm was used to find the best controls matches for each case. A Love plot was used to show the covariate balance. Conditional logistic regression were used to evaluate the association between outcomes and emergency surgery on the matched sample.
Results
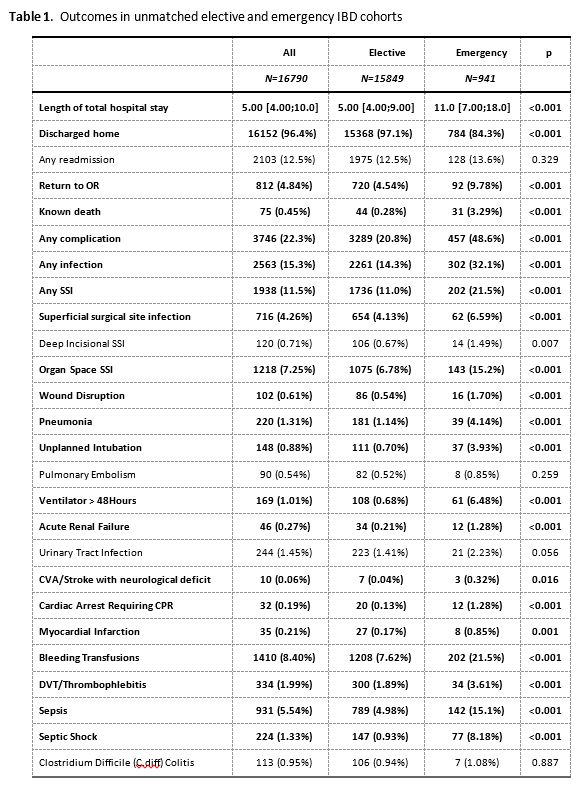
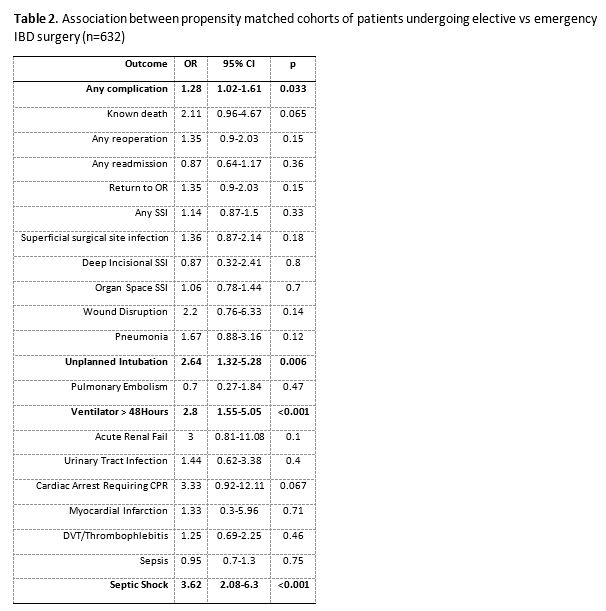
A total of 16,790 patients (15,849 elective, 941 emergency) were included in the unmatched cohort analysis. 30-day outcomes in 21 categories including length of stay, surgical site infection, sepsis, death and cardiovascular, renal and thrombotic complications were worse in the emergency cohort (Table 1). After matching, 632 sets were constructed. The majority of adverse outcomes demonstrated in the unmatched cohort lost significance. Only unplanned intubation (OR 2.6, p=.006), >48 hours on a ventilator (OR 2.8, p<.001), septic shock (OR 3.6, p<.001) and any complication (OR 1.3, p=.03) retained significance (Table 2).
Conclusion
In concordance with the current literature, we demonstrated increased rates of postoperative infection, cardiovascular and renal complications, reoperation and length of stay in unmatched groups of IBD patients undergoing emergency vs elective surgery. However, the majority of these complications were not significantly different after propensity matching. This suggests that emergency surgery is not associated with poorer outcomes in terms of length of stay, mortality and most morbidities as previously thought.


