P235 Patients with inflammatory ileal pouch anal anastomosis (IPAA) disorders are characterized by a distinct breath volatile organic compounds (VOC) metabolome profile
Qazi, T.(1)*;Ottichilo, R.(2);Grove, D.(2);Rayan, C.(2);Cohen, B.(1);Bhat, S.(3);Regueiro, M.(1);Dweik, R.(4);Rieder, F.(1);
(1)Digestive Disease and Surgery Institute, Department of Gastroenterology- Hepatology and Nutrition, Cleveland, United States;(2)Lerner Research Institute, Department of Inflammation and Immunity, Cleveland, United States;(3)Digestive Disease and Surgery Institute, Department of Gastroenterology- Hepatology and Nutrition, Twinsburg, United States;(4)Respiratory Institute, Allergy and Immunology- Critical Care Medicine- and Infectious Disease, Cleveland, United States;
Background
Following creation of an IPAA in patients with ulcerative colitis (UC), more than 60% of subjects develop inflammatory complications. The current objective assessment for inflammation of the pouch is limited to surrogate stool and blood biomarkers or endoscopy. The development of non-invasive and accurate biomarkers for the assessment of IPAA inflammation is an area of unmet need. Measurement of exhaled breath volatile organic metabolome compounds (VOCs) has shown promise as a biomarker for the diagnosis and monitoring of inflammatory disorders. We here aimed to characterize the pattern of VOCs in the exhaled breath of patients with an IPAA and assess whether VOC analysis is able to discriminate patients with endoscopically active IPAA inflammation from patients without IPAA inflammation.
Methods
This is a cross-sectional study of patients with an IPAA created for the management of UC. Exhaled breath samples were collected at time of endoscopic evaluation of the pouch and 97 VOC metabolites assessed via selective ion flow tube mass spectrometry (SIFT-MS). The IPAA cohort was dichotomized using the endoscopic pouch disease activity index (PDAI) into endoscopic PDAI of >= 4 (severe inflammation), or endoscopic PDAI score <= 1 (mild or no inflammation). Principle component analysis (PCA) was conducted to reveal the VOCs with the strongest discriminatory capability and principle component regression (PCR) was performed to assess the association of exhaled breath VOC analysis in differentiating the groups.
Results
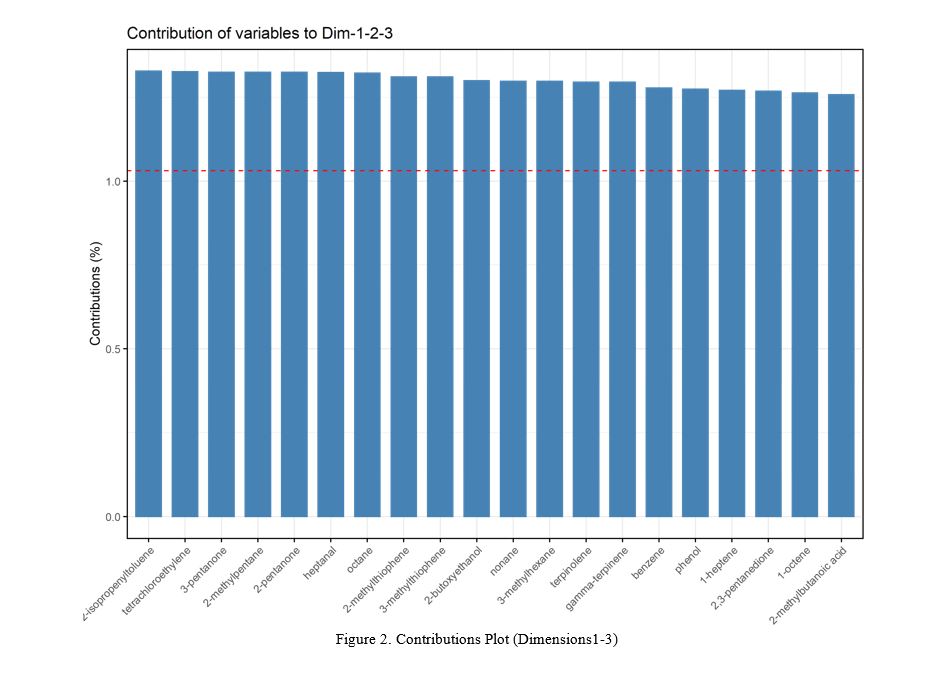
Exhaled breath metabolome analysis was performed on 10 subjects with PDAI >=4 and 7 subjects with PDAI <=1. Demographics are provided in Table 1. PCA indicated robust discrimination of the two groups based on breath VOCs (Figure 1). 10 out of 97 VOCs were up-regulated in the PDAI >=4 group compared to control, including ammonia and hydrogen sulfide. Isopropenyltoluene, tetrachloroethylene, and 3-pentanone provided the highest contribution to differentiate between the cohorts (Figure 2). Receiver operative curve (ROC) analysis of the PCR model indicated an area under the curve (AUC) of 0.81 (0.61-99), suggesting a strong association of breath VOCs with inflammation of the pouch (Figure 1).
Conclusion
VOC exhaled breath metabolome analysis shows a strong ability to discriminate patients with severe endoscopic pouch inflammation from patients with minimal to no endoscopic inflammation. The differences in reported VOCs point toward metabolic differences in bacterial fermentation, lipid and carbohydrate metabolism, and an increase in reactive oxygen species in patients with endoscopic pouch inflammation. Validation studies addressing the role of VOC analysis for non-invasive disease assessment patients with IPAA are ongoing.