P235 Serological biomarkers of interstitial matrix and basement membrane remodelling correlate the Modified Mayo Endoscopic Score (mMES) for ulcerative colitis
J. Mortensen1, L.E. Godskesen2, M. Lindholm1, A. Krag2, M.A. Karsdal1, T. Manon-Jensen1, J. Kjeldsen2
1Nordic Bioscience A/S, Biomarkers and Research, Herlev, Denmark, 2Department of Gastroenterology and Hepatology, Odense University Hospital, Odense, Denmark
Background
Endoscopy is a mainstay in ulcerative colitis (UC) for disease activity monitoring. The modified Mayo Endoscopic Score (mMES) for UC takes into account disease extent and hereby additional objectivity can be achieved for endoscopic assessment. However, endoscopic evaluation of the intestinal mucosa is time-consuming and inconvenient for the patients. Therefore, surrogate biomarkers for endoscopic examinations are warranted. The aim of this study was to evaluate serological neo-epitope biomarkers of type IV collagen degradation (C4M) and formation (PRO-C4), type III collagen degradation (C3M), type V collagen formation (PRO-C5) and macrophage activity (VICM) and their association with the mMES for UC.
Methods
Endoscopic disease activity was scored using mMES for UC patients (
Results
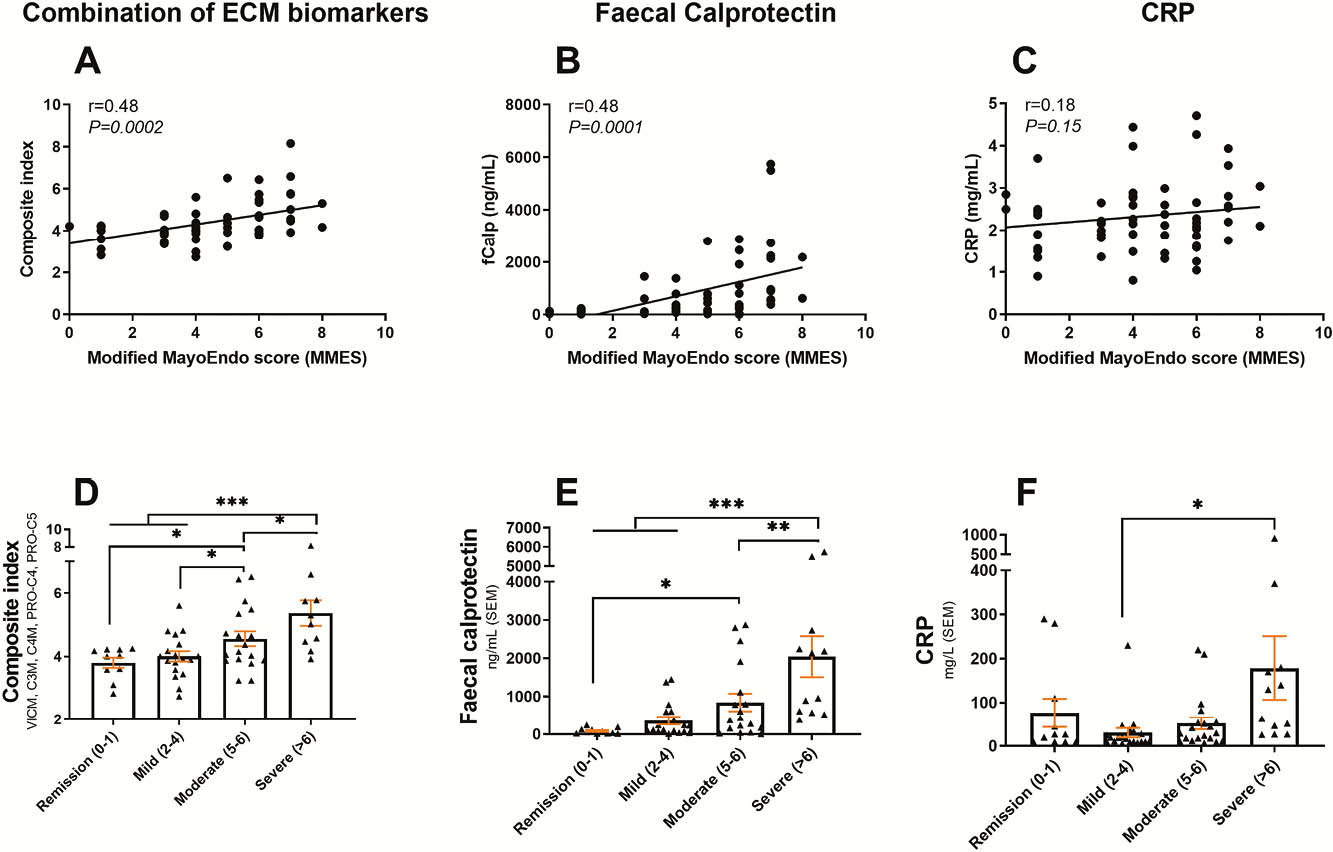
All the biomarkers correlated to mMES (VICM:
Conclusion
The combined tissue-remodelling biomarkers correlated significantly with mMES for UC. The ECM serological biomarkers performed better than CRP, and equally good as FC. Thus, serological biomarkers of ECM remodelling, especially basement membrane degradation, interstitial matrix degradation and macrophage activity biomarkers may be used as surrogate markers for endoscopic disease activity assessment for UC.


