P239 Incidence of Long COVID and impact of medications on the risk of developing Long COVID in a nationwide cohort of Inflammatory Bowel Disease patients
Khan, N.(1,2)*;Mahmud, N.(1,2);Patel, M.(1);Sundararajan, R.(1);Reinisch, W.(3);
(1)Corporal Michael J Crescenz VA Medical Center, Gastroenterology, Philadelphia, United States;(2)University of Pennsylvania- Perelman School of Medicine, Gastroenterology, Philadelphia, United States;(3)Medical University of Vienna, Gastroenterology, Vienna, Austria;
Background
With the ongoing SARS-CoV-2 pandemic there is concern for development of Long COVID in patients with immune-mediated diseases treated with immunosuppressive agents. We aimed to determine the incidence of Long COVID among Inflammatory Bowel Disease (IBD) patients and to identify associated risk factors. Our study also aimed at studying the differences in risk of Long COVID among different IBD medication exposures.
Methods
We conducted a retrospective cohort study utilizing a nationwide cohort of patients with IBD in the Veteran Affairs Healthcare System (VAHS). Patients diagnosed with SARS-COV-2 between March 10th, 2020, and January 24th, 2021, were included. All charts were reviewed to determine recent IBD hospitalization, hospitalization for SARS-CoV-2 infection, and stability of IBD control pre and post infection. COVID-19 hospitalizations were also reviewed for intensive care unit requirement (ICU). COVID-19 treatments including remdesivir, monoclonal antibody infusions, and corticosteroids were also ascertained. Primary outcome was development of Long COVID. Cox regression analysis was used to identify variables associated with Long COVID.
Results
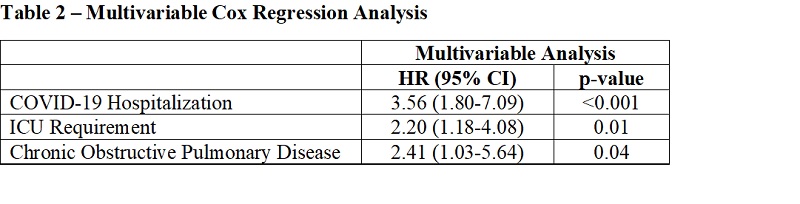
A total of 677 patients with SARS-CoV-2 infection were included, of which 49 (7.3%) were diagnosed with Long COVID (Table 1). No significant differences in IBD medication class between patients with and without Long COVID diagnoses were noted. In multivariable regression analysis, COVID-19 hospitalization (HR 3.56, 95% CI 1.80-7.09, p<0.001), ICU requirement (HR 2.20, 95% CI 1.18-4.08, p=0.01), and COPD (HR 2.41, 95% CI 1.03-5.64, p=0.04) were significantly associated with Long COVID (Table 2). Adjusted survival curves showed that relative to patients who were not hospitalized, patients hospitalized in the ICU had an 8.61-fold increased hazard of Long COVID (HR 8.61, 95% CI 3.98-18.65, p<0.001) (Figure 1).
Conclusion
Hospitalization and ICU care for COVID-19, as well as pre-existing COPD, were associated with increased risk of developing Long COVID, suggesting that severity of infection with a vulnerable substrate are key drivers of risk. Medications used in the treatment of IBD did not impact the risk of Long COVID. These findings should help reassure and inform IBD patients about the risk of Long COVID.