P247 Oncostatin M and its receptor are markers of endoscopic and histological disease activity in Inflammatory Bowel Disease
Nguyen, A.(1,2)*;Sturm, G.(3);Plattner, C.(3);Trajanoski, Z.(3);Atreya, R.(4);IBDome Consortium, I.C.(2,3,4);Siegmund, B.(2);Hegazy, A.N.(2,5,6);
(1)Monash University, Central Clinical School, Melbourne, Australia;(2)Charité – Universitätsmedizin Berlin- corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Medical Department of Gastroenterology- Infectiology and Rheumatology, Berlin, Germany;(3)Medical University of Innsbruck, Biocenter- Institute of Bioinformatics, Innsbruck, Austria;(4)Friedrich-Alexander-Universität, Medizinische Klinik 1- Universitätsklinikum Erlangen, Erlangen-Nürnberg, Germany;(5)Charité – Universitätsmedizin Berlin, Berlin Institute of Health BIH, Berlin, Germany;(6)German Rheumatism Research Center DRFZ- a Leibniz Institute, Inflammatory Mechanisms, Berlin, Germany; IBDome Consortium
Background
Oncostatin M (OSM) and its receptor (OSMR) have been associated with active disease in patients with inflammatory bowel disease (IBD). This study compared the expression of OSM and OSMR in intestinal tissue according to clinical, endoscopic, and histological disease activity.
Methods
A multi-centre IBD database containing RNA-sequencing datasets, was used to analyse OSM and OSMR expression in ileal and/or colonic tissue, expressed as transcripts per million (TPM). Clinical scoring systems included the Harvey Bradshaw Index for Crohn’s disease (CD) and partial Mayo score for ulcerative colitis (UC). Endoscopic scoring systems included the simple endoscopic score for CD (SES-CD) and UC endoscopic index of severity (UCEIS). Histological scoring included the modified Naini and Cortina, and Riley scores. Graphs were presented in log transformed TPM+1 values.
Results
155 patients (108 CD, 47 UC) and 38 controls were included. For IBD patients, 49% were men, median age was 35 years and intestinal tissue was collected at endoscopy (73%) and surgery (27%). Compared to controls, patients with CD and UC had significantly elevated median expression of OSM (0.08, 0.29 and 0.34 TPM respectively) and OSMR (1.21, 1.69 and 3.53 TPM respectively). OSMR expression was higher in UC patients than CD (p<0.001). There was no difference in OSM or OSMR between Harvey Bradshaw Index categories (0-4 vs 5-7 vs 8-16) or partial Mayo scores (0 vs 1-3 vs 4-7). Endoscopically, OSM was higher for SES-CD scores of 16-51 (1.11 TPM), compared to SES-CD scores of 0-3 (0.14 TPM, p=0.003) and controls (0.08 TPM, p<0.0001). Median OSMR increased non-significantly with increasing SES-CD scores (score 0-3: 1.59 TPM; score 4-15: 1.90 TPM; score 16-51: 2.04 TPM). There was no difference in OSM and OSMR expression between UCEIS scores, but the most severe disease (UCEIS score 5-8) had higher expression than controls for both OSM (3.92 vs 0.08 TPM, p<0.001) and OSMR (6.10 vs 1.21 TPM, p<0.0001). Increasing expression of OSM and OSMR was found with increasing histological scores, see Figure. Using the modified Naini and Cortina score for CD, OSM and OSMR were most expressed in the highest scores compared to the lowest scores (OSM: 1.48 vs 0.09 TPM, p<0.001; OSMR: 5.50 vs 1.27 TPM, p=0.003). For the modified Riley score for UC, both OSM and OSMR were also able to differentiate between the highest and lowest score groups (OSM: 3.14 vs 0.12 TPM, p=0.0001; OSMR: 6.61 vs 1.58 TPM, p<0.0001). 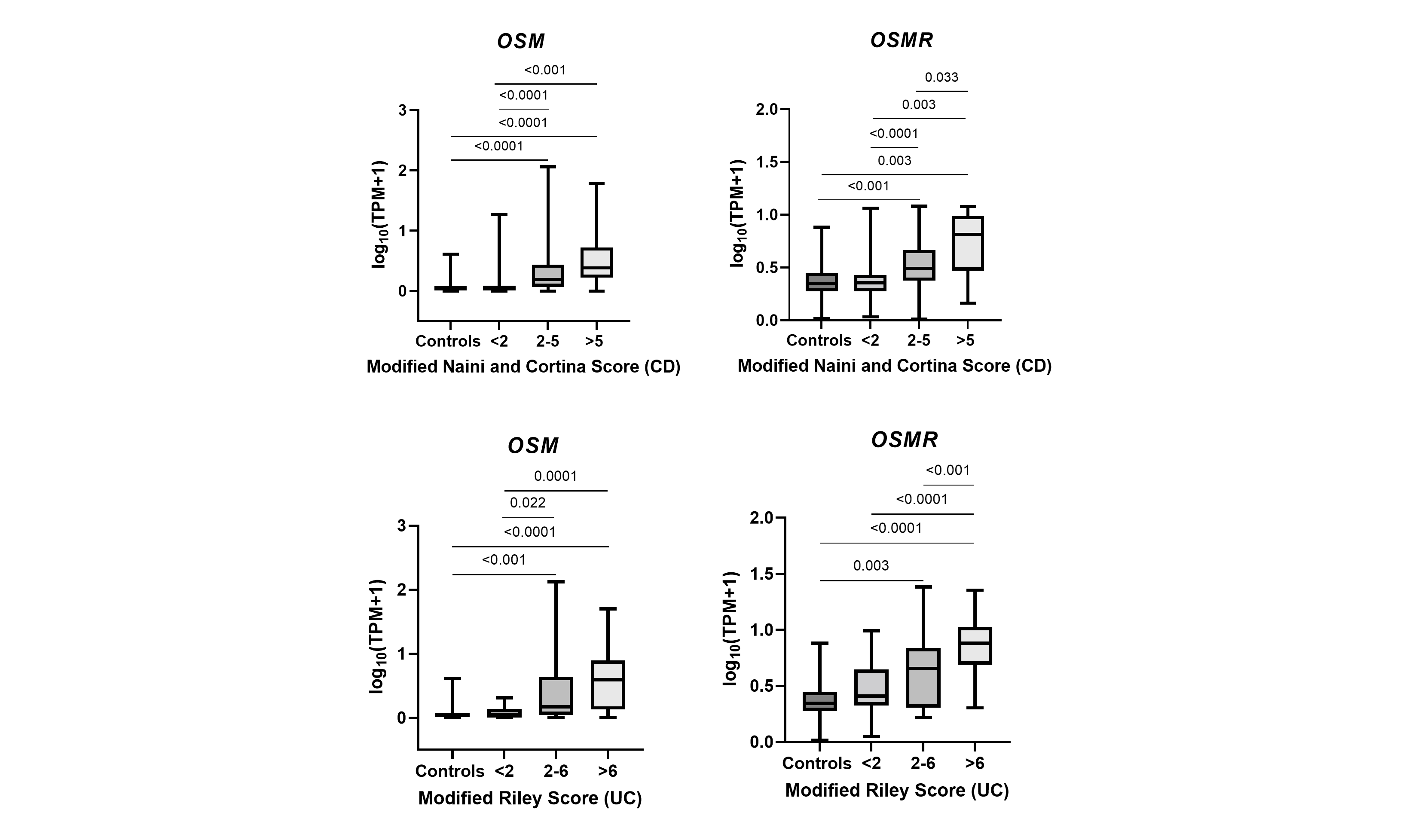
Conclusion
This study showed that OSM and OSMR expression in intestinal tissue is associated with inflammation both histologically and endoscopically. Further investigations are needed to confirm our observations and explore the OSM pathway’s relevance in intestinal inflammation.


