P255 Predictors of postoperative morbidity in patients with inflammatory bowel disease
N. Imperatore, L. Pellegrini, L. Bucci, A. Rispo, A.D. Guarino, A. Testa, R. Peltrini, A. Amendola, M. Patturelli, F. Castiglione
Federico II University of Naples, Department of Clinical Medicine- Gastroenterology and Surgery, Naples, Italy
Background
More than half of patients suffering from inflammatory bowel disease (IBD) requires surgery in their lifetime. However, predictors of post-operative morbidity and mortality are poorly investigated. Our aim was to assess the predictors of post-operative mortality and morbidity in IBD.
Methods
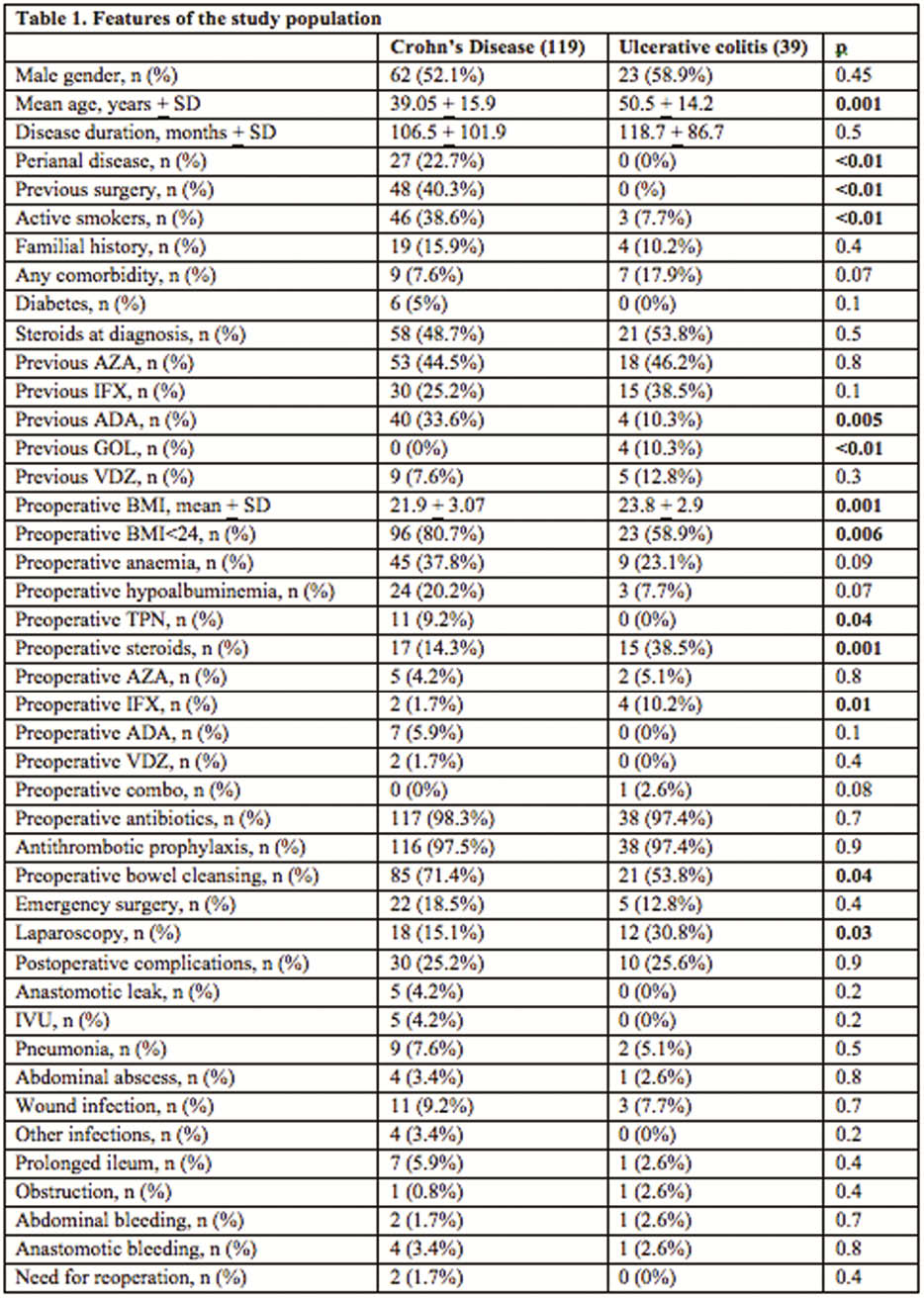
retrospective cohort study enrolling all IBD subjects followed-up and operated at our tertiary IBD Centre from 2015 to 2018. For each patient, we evaluated patient-dependent (comorbidities, smoking, drugs, nutritional status), disease-dependent (disease duration, location, behaviour, extension), surgery-dependent variables (duration, emergency/election, laparoscopy/laparotomy, bowel/colic resection, length of intestinal resection).
Results
158 subjects were operated during the period study (males 53.8%, Crohn’s disease 75.3%, mean age 41.9 + 16.2, disease duration 109.5 + 98.3 months); the majority (83%) underwent an elective surgery. No patient died. About morbidity, 40 (25.3%) developed post-operative complications: wound infection (8.9%), respiratory complications (6.9%), prolonged ileum (5.1%), anastomotic leak (3.2%), urinary infections (3.2%), abdominal abscess (3.2%), anastomotic bleeding (3.2%), other infections (2.5%), abdominal bleeding (1.9%), obstruction (1.3%). Two subjects (1.3%) required re-operation within 30 days. A surgery-duration <142 min was predictive for a better post-operative outcome (sensitivity 80%, specificity 42%, PPV 32%, NPV 85.9%). At binary logistic regression, stricturing/fistulizing behaviour (OR 3.7, 95% CI 1.6–6.4,
Conclusion
about a quarter of IBD patients undergoing surgery develops a post-operative complication, especially infective. Several patient-related, disease-related and surgery-related factors are predictive for post-operative morbidity. The recognition of these factors, as well the multidisciplinary approach (gastroenterologists, surgeons and nutritionists), and intensive preoperative management could be able to minimise these complications.


