P260 Autoimmune pancreatitis in patients with Inflammatory Bowel Disease: results from a multicentre ECCO CONFER cases series
Eder, P.M.(1);Verstock, B.(2);Culver, E.(3);Dragoni, G.(4);Kredel, L.I.(5);de Paredes, A.G.G.(6);Kaniewska, M.(7);Leibovitzh, H.(8);Oracz, G.(9);Ribaldone, D.G.(10);Wypych, J.(11);Badaoui, A.(12);Rahier, J.F.(12);Bezzio, C.(13);Bossuyt, P.(14);Falloon, K.(15);Vozzo, C.F.(15);Jess, T.(16);Larsen, L.(17);Olensen, S.S.(18);Starzyńska, T.(19);Chaparro, M.(20);Dror, D.(21);Ellul , P.(22);Gromny, I.(23);Maciejewska, K.(7);Peleg, N.(24);Shitrit, A.B.G.(25);Szwed, Ł.(26);Talar-Wojnarowska, R.(27);Snir, Y.(28);Zittan, E.(29);Goren, I.(30);
(1)Poznan University of Medical Sciences, Department of Gastroenterology- Dietetics and Internal Medicine, Poznań, Poland;(2)University Hospitals Leuven- KU Leuven, Department of Gastroenterology and Hepatology. Department of Chronic Diseases and Metabolism., Leuven, Belgium;(3)John Radcliffe Hospital Oxford, Translational Gastroenterology Unit, Oxford, United Kingdom;(4)Careggi University Hospital, Department of Gastroenterology, Florence, Italy;(5)Charité-Universitätsmedizin Berlin, Division of Gastroenterology- Infectiology and Rheumatology- Medical Department, Berlin, Germany;(6)Hospital Universitario Ramon y Cajal. Universidad de Alcala. IRYCIS., Gastroenterology and Hepatology Department, Madrid, Spain;(7)Central Clinical Hospital of Ministry of Internal Affairs, Department of Internal Medicine and Gastroenterology with IBD Subdivision, Warsaw, Poland;(8)Temerty Faculty of Medicine- Mount Sinai Hospital- University of Toronto, Zane Cohen Centre for Digestive Diseases- Division of Gastroenterology & Hepatology, Toronto, Canada;(9)The Children’s Memorial Health Institute, Department of Gastroenterology- Hepatology- Feeding Disorder and Pediatrics, Warsaw, Poland;(10)University of Turin, Department of Medical Sciences, Turin, Italy;(11)Copernicus Hospital, Department of Gastroenterology- Surgery and Nutrition, Gdańsk, Poland;(12)Université Catholique de Louvain, Department of Gastroenterology- CHU UCL Namur, Yvoir, Belgium;(13)Rho Hospital, Gastroenterology Unit, Rho Milano, Italy;(14)Imelda General Hospital, Imelda GI Clinical Research Center, Bonheiden, Belgium;(15)Digestive Diseases and Surgery Institute- Cleveland Clinic, Department of Gastroenterology- Hepatology and Nutrition, Cleveland, United States;(16)Aalborg University, Center for Molecular Prediction of Inflammatory Bowel Disease- Department of Clinical Medicine, Aalborg, Denmark;(17)Aalborg University Hospital and Aalborg University, Department of Gastroenterology and Hepatology. Center for Molecular Prediction of Inflammatory Bowel Disease – PREDICT- Department of Clinical Medicine- The Faculty of Medicine., Aalborg, Denmark;(18)Aalborg University Hospital and Aalborg University, Centre for Pancreatic Diseases and Mech-Sense- Department of Gastroenterology and Hepatology. Department of Clinical Medicine, Aalborg, Denmark;(19)Pomeranian Medical University in Szczecin, Department of Gastroenterology, Szczecin, Poland;(20)Hospital Universitario de La Princesa- Instituto de Investigación Sanitaria Princesa IIS-IP, Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas CIBEREHD, Madrid, Spain;(21)Galilee Medical Center, Department of Gastroenterology, Nahariya, Israel;(22)Mater dei Hospital, Division of Gastroenterology, Msida, Malta;(23)Wroclaw Medical University, Department of Gastroenterology and Hepatology, Wrocław, Poland;(24)Rabin Medical Center, The Division of Gastroenterology, Petah Tikva, Israel;(25)The Hebrew University of Jerusalem- Shaare Zedek Medical Center, IBD MOM Unit- Digestive Diseases Institute, Jerusalem, Israel;(26)Private Gastroenterology Practice, Private Gastroenterology Practice, Nowy Dwór Mazowiecki, Poland;(27)Medical University of Lodz, Department of Digestive Tract Diseases, Łódź, Poland;(28)Rabin Medical Center- Beilinson Campus, Gastroenterology Division, Petah Tikva, Israel;(29)Emek Medical Center, Ellen and Pinchas Mamber Institute of Gastroenterology and Liver Diseases- IBD Unit, Afula, Israel;(30)Rabin Medical Center affiliated with Sackler Faculty of Medicine- Tel Aviv University IL. Lerner Research Institute- Cleveland Clinic US., Division of Gastroenterology IL. Department of Inflammation and Immunity US., Petah Tikva IL. Cleveland US., Israel;
Background
Autoimmune pancreatitis (AIP) is an uncommon inflammatory disorder that may accompany inflammatory bowel disease (IBD). The clinical relevance of AIP-IBD coexistence, therapeutic strategies, and long-term outcomes are scarcely known.
Methods
In this ECCO COllaborative Network For Exceptionally Rare case reports project (ECCO-CONFER) we included cases of AIP diagnosed in patients with IBD. Data on the diagnostic criteria, clinical characteristics, and patient outcomes were retrospectively collected and analysed.
Results
The cohort included 82 patients [54% males, 77% with ulcerative colitis (UC), age at IBD and AIP diagnosis 32±16 and 35±16 years, respectively]. Of all AIP patients, 71% were classified as type 2, 21% as type 1, and 8% as undefined type. Detailed characteristics of the study group are shown in Table 1. In 57% of the individuals, IBD was diagnosed before AIP. In the remaining cases, IBD was diagnosed simultaneously (20%) or afterwards (23%). Half of the patients required immunomodulators and 43% biological therapy to control their IBD. Twenty-two percent of UC and 6% of Crohn’s disease (CD) required surgical intervention during a mean follow-up of 3.6±3.4 years. Histological confirmation was used in 38% of cases, while the remaining were diagnosed as probable AIP based on clinical, biochemical, and radiologic criteria. Magnetic resonance was the most frequently used imaging modality (61%). Eighty percent of patients received steroids for AIP. Thiopurines were used for AIP in 16 (19%) patients, 81% of them responded to treatment. One patient was successfully treated for AIP with infliximab. AIP complications occurred in 27%, including pancreatic exocrine insufficiency (19%) and diabetes (13%). Five patients underwent surgery due to suspected pancreatic cancer. Patients with complicated AIP were significantly older at AIP and IBD diagnosis, were more frequently males and presented with weight loss at AIP diagnosis, and had less frequently a family history of IBD (Table 1). Colonic IBD (i.e. UC, isolated colonic IBD-unclassified or colonic CD) was seen in a higher proportion of individuals with complicated vs benign AIP course (91% vs 33%, p<0.0001). At the end of follow-up, 75 (91%) and 73 (89%) patients were in remission of AIP and IBD, respectively. No IBD or AIP-related deaths were reported. 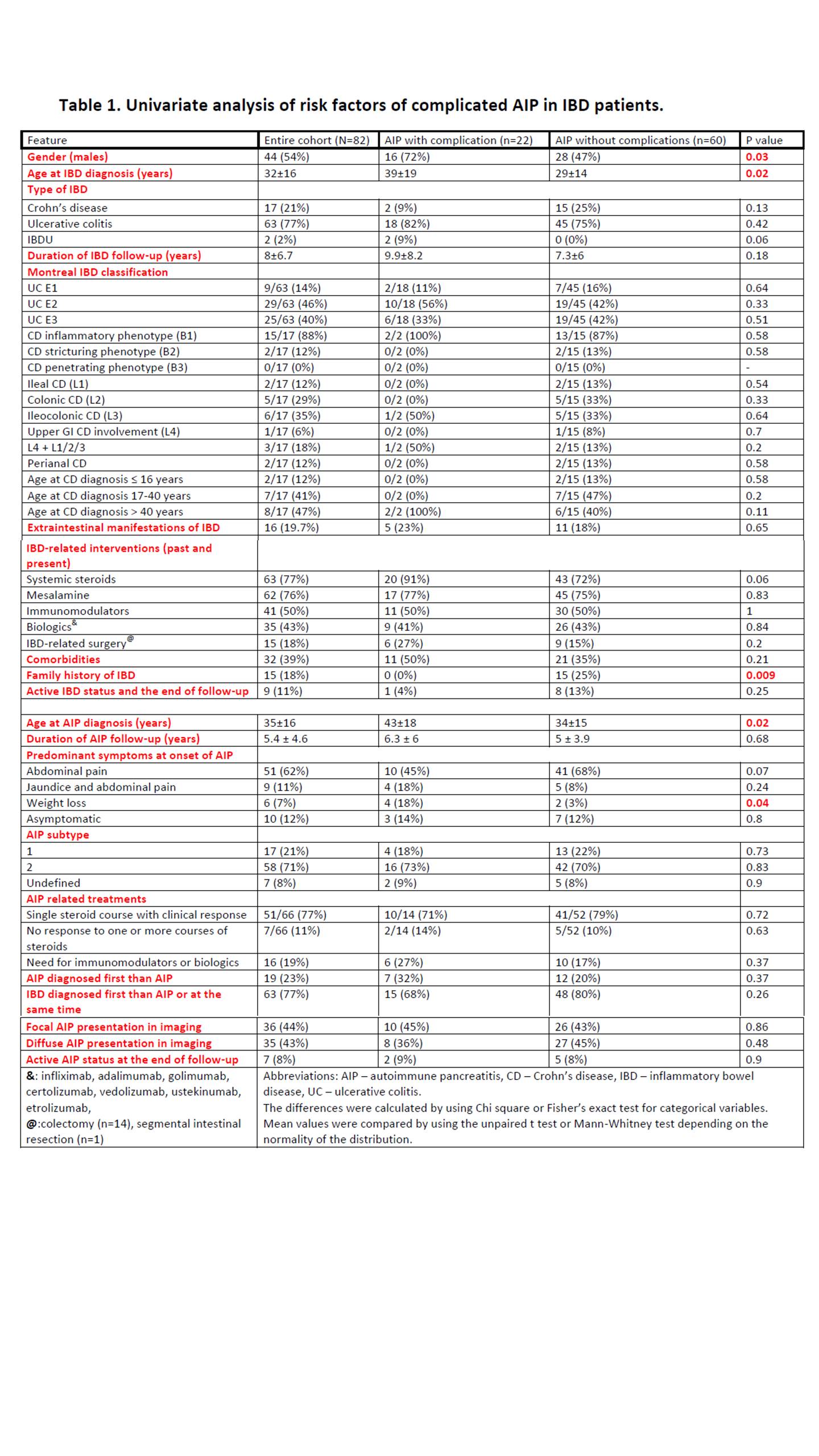
Conclusion
In this large international cohort of patients with concomitant AIP-IBD, most patients have type 2 AIP and colonic IBD. AIP course is relatively benign, and long-term outcomes are favourable. Older age, male gender, isolated colonic IBD location, and weight loss at AIP presentation were seen in higher proportions of patients with a complicated course of AIP.


