P262 Trends in the prevalence and severity of anaemia in paediatric patients with inflammatory bowel disease in the last decade
S.Y. Geng, Z. Ridha, B.L. Pham, E. Tran, A. Peixoto, S.A. Tchogna, C. Deslandres, P. Jantchou
The Sainte-Justine University Hospital Centre, Department of Pediatric Gastroenterology, Montréal, Canada
Background
Anaemia is one of the most common extraintestinal manifestations in patients with inflammatory bowel disease(IBD) at diagnosis. Studies have shown that anaemia was associated with low levels of quality of life, which improves with the correction of anaemia in adults. Recent data have shown an increase in the incidence and severity of paediatric IBD. We aim to investigate the trends in the prevalence of anaemia in children at diagnosis of IBD in the last decade. The secondary aim was to investigate the associations between haemoglobin (Hb) levels and disease characteristics.
Methods
Eligible patients (age ≤18 years, diagnosed with IBD from 2009 to 2018) were retrospectively identified through a prospective IBD database maintained at CHU Sainte-Justine, Montreal, Canada. Disease localisation and phenotype were defined according to the Paris Classification of IBD. Anaemia was defined by Hb levels according to WHO targets. The annual prevalence of anaemia was calculated according to subtype (inflammatory vs. iron deficiency). The Pediatric Crohn’s Disease Activity Index(PCDAI) and the Pediatric ulcerative colitis Activity(PUCAI) Index were used to assess the disease severity at diagnosis.
Results
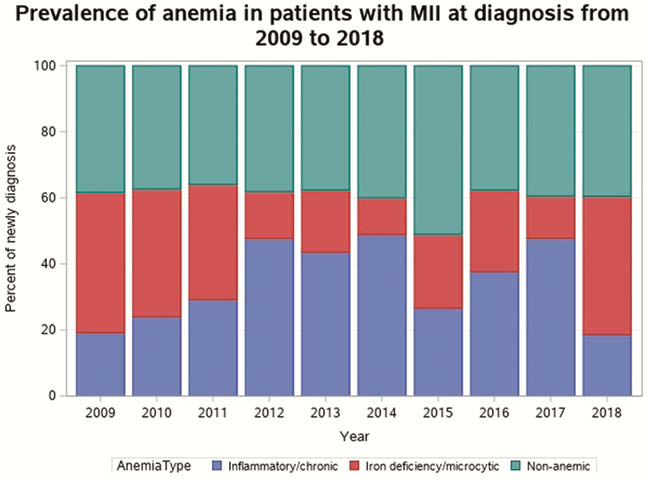
We included 887 patients (439 females), mean(SD) age of 13.1 (3.4) years. Of these, 519 (58.5%) were identified with anaemia within 30 days of diagnosis. The median (IQR) Hb level at diagnosis was 108 (98 −114) g/dl. Severe anaemia(< 70 g/dl) was present in 1.8 % of patients. The prevalence of anaemia at diagnosis remained relatively stable ranging from 60.2% in 2009 to 60.4% in 2018. The annual proportion of inflammatory vs. iron-deficiency anaemia is displayed in Figure 1. Anaemia was more prevalent in CD (62.2%) than UC (57.9%) or IBD-U(39.6%). The median(IQR) PCDAI and PUCAI were respectively 37.5 (27.5–47.5) and 55.0 (40.0–65.0) in the anaemic group as compared with 27.5 (20.0–37.50) and 35.0 (25.0–55.0) in the non-anaemic group;
Conclusion
Anaemia remains a prevalent symptom in paediatric patients with IBD, and it is correlated with the extent of intestinal involvement and disease severity. The impact of anaemia at diagnosis and during follow-up on the levels of quality of life and physical activity is currently under investigation.


