P283 Awareness and perceptions of colorectal cancer risk and screening in Inflammatory Bowel Disease
Liu, E.(1)*;Erande, A.(2);McLaughlin, J.(3);Limdi, J.K.(1);
(1)The Northern Care Alliance NHS Trust, Department of Gastroenterology- Section of IBD, Bury- Manchester, United Kingdom;(2)Metropolis Healthcare, Metropolis, Mumbai, India;(3)University of Manchester, Division of Diabetes Endocrinology and Gastroenterology, Manchester, United Kingdom;
Background
Patients with inflammatory bowel disease (IBD) are at higher risk of developing colorectal cancer (CRC). Guidelines recommend periodic endoscopic surveillance to detect and manage dysplasia. We aimed to explore patient knowledge and perceptions of CRC risk and colonoscopic surveillance and identify potential barriers to surveillance practice.
Methods
A 44-item questionnaire was administered to IBD patients with colonic involvement attending gastroenterology clinics between July 2021 and April 2022.
Results
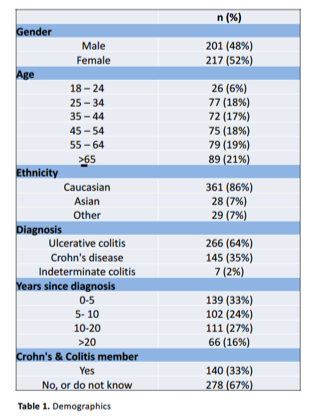
Of 418 respondents (demographics see table 1), 266 (64%) had ulcerative colitis and 145 (34%) had Crohn’s disease, with 177 (42%) diagnosed for ≥10 years. Two hundred and sixty-five (66%) patients rated their IBD control moderate/good (score ≥7/10), and 314 (75%) self-rated their understanding of IBD as good/excellent. Two hundred and ninety-eight patients (71%) recognised that CRC risk is higher in IBD but 83 (20%) felt the risk of CRC was lower in IBD or were unsure. Age (p=0.02), being a Crohn’s and Colitis UK (CCUK) member (p<0.001), patient rated IBD control (p=0.04) and self-rated understanding of IBD (p=0.01) were associated with better CRC risk awareness. One hundred and forty-nine (36%) respondents stated that their IBD healthcare professional (HCP) had previously discussed CRC risk with them; this was associated with better CRC knowledge (p=0.001). On multivariate analysis CCUK membership (OR 2.75; 95% CI 1.57- 4.83; p<0.001), prior HCP discussion (OR 1.57; 95% CI 0.85-2.87; p=0.01) and age ≥65 years (OR 0.3; 95% CI 0.09- 0.99; p=0.05) were predictive of greater CRC risk awareness. Concerning the most appropriate screening test for dysplasia, 369 patients (88%) stated colonoscopy, but only 29 (7%) were aware that colonic surveillance should commence 8-10 years after diagnosis; 153 (37%) recognised that optimal timing is when IBD is in remission. Patient reported information sources included gastroenterology HCPs (43%), patient support groups (28%), and patient leaflets (17%). The majority (78%) stated they would agree to have surveillance colonoscopy if advised by their HCP. Bowel preparation (50%) and discomfort (45%) were factors most likely to dissuade patients from agreeing to surveillance.
Conclusion
Patient knowledge of CRC risk and surveillance practice in IBD is variable. Modifiable factors associated with improved knowledge are discussion with HCPs and CCUK membership. Our findings underscore the need for better patient education to aid informed decision-making between patients and HCPs and improve adherence to colonoscopic surveillance.


